October 15, 2013 (Vol. 33, No. 18)
The development of multiplex companion diagnostics is driven by the need to understand efficacy and safety at both the molecular and phenotypic levels. In the future, personalized therapeutic regimens will be tailored to each patient’s genomic, transcriptomic, and epigenomic profiles to optimize individual outcomes.
For personalized (or precision) medicine to become a sustaining reality, all stakeholders—patients, healthcare professionals, drug development companies, regulatory agencies and payers—must work together.
Advancing multiplex companion diagnostics technology was among the topics discussed at CHI’s “Next Generation Diagnostics Summit,” an event held recently in Washington, DC.
“Pharmaceutical companies are more comfortable today with the value of using a personalized medicine approach in their drug discovery and development programs,” explained Jeremy Bridge-Cook, Ph.D., senior vp of research and development at Luminex.
“Reimbursement changes and inconsistencies constrained the market in 2013 and will need to be sorted out, or personalized medicine and its ability to deliver substantial healthcare savings will be slowed down dramatically.”
Rather than being the exception, companion diagnostics are becoming the norm in oncology. In other clinical areas, such as chronic and infectious diseases, advancements in biomarker programs are also being made. Many of these programs are at an earlier stage, however, with some just entering clinical trials.
Multiplex assays mitigate patient risk. For example, approximately a quarter of the drugs used clinically today are metabolized by cytochrome P450 2D6. The Luminex xTAG® CYP2D6 Kit v3 can be used as a clinical aid in determining therapeutic strategy. The qualitative genotyping assay analyzes 20 different cytochrome P450 2D6 variants and identifies metabolic differences, which can be used to help evaluate the risk of adverse events.
Another challenging syndrome is Alzheimer’s disease. Most of the damage caused by Alzheimer’s disease happens subclinically, before clinical symptoms emerge. Already a big problem, Alzheimer’s disease will become a larger problem as baby boomers age and become more susceptible.
The use of a biomarker test for earlier diagnosis is thought by many to be a better way to demonstrate efficacy of a drug for halting Alzheimer’s progression. Luminex and Merck recently announced a partnership around a companion diagnostic for an Alzheimer’s disease compound in development.
Reimbursement remains an issue. Increasingly, evidence based on healthcare economic trials will be required to prove that a precision medicine approach reduces healthcare system costs.
Clinical trials demonstrate clinical outcomes. Healthcare economic trials are essentially the same activity, except that outcomes are measured in economic, not clinical, factors. Standard cost of care is compared to the cost of a personalized approach, that is, a model in which a companion diagnostic is followed by a precision therapeutic.
“Healthcare economic trials have been implemented for some time—just not for companion diagnostics. The industry as a whole is still learning, and although there is a pilot program in its infancy between the FDA and CMS, there is no set protocol,” concluded Dr. Bridge-Cook.
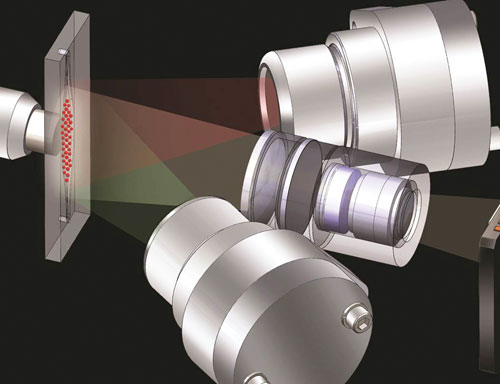
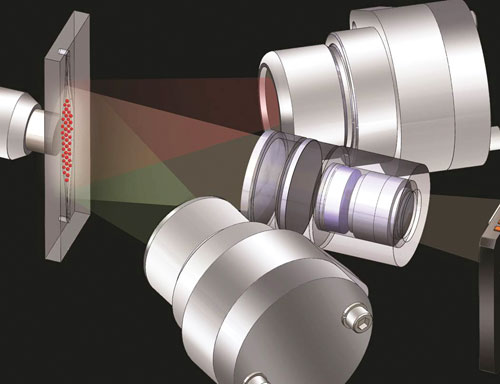
Luminex microspheres pass through a red laser or LED, which excites the internal dyes to distinguish the microsphere set. Then a green laser or LED, which excites the fluorescent dye on the reporter molecule, determines the result of the assay.
A Multiplex Microfluidics Platform
A fully integrated microfluidics platform for molecular diagnostics is currently available from Rheonix. Intended for research use, the platform is composed of the EncompassMDx™ instrument and a disposable CARD® Consumable cartridge. The cartridge contains all necessary pumps, valves, and reagent and reaction reservoirs.
Software delivers pneumatic signals to the cartridge to move fluids throughout the device and perform all processing steps including cell lysis, DNA or RNA extraction and purification, multiplex PCR amplification, and detection in either an end-point or real-time manner. FDA approval is expected in 2014.
A variety of multiplex assays can be performed on the platform, including pharmacogenomics tests for warfarin and Plavix sensitivity, a test for four common sexually transmitted infections, and a PCR assay to detect and distinguish 20 clinically relevant human papillomavirus (HPV) subtypes.
In addition, a “dual assay” can simultaneously perform both an immunoassay and PCR-based assay for the detection of HIV-1 in saliva samples. An aqueous-based system allows processing and analysis of FFPE samples.
“FFPE tumor blocks are a valuable resource. Now, you can take a curl, put it into the CARD, push ‘go,’ and get results. The CARD introduces the aqueous-based buffer to remove the paraffin and reverse the cross-linking. The cells are lysed, and the rest of the steps are the same as our other assays,” said Richard A. Montagna, Ph.D., senior vp for corporate business development and scientific affairs, at Rheonix.
“That would have taken a lot of expense and work on the benchtop. Results show that we are now detecting seven different somatic cell mutations involving the KRAS colon cancer marker in FFPE tumor blocks,” added Dr. Montagna. “Our mandate is not to just do good science, but to do it in a manner that permits larger-scale, cost-effective manufacturing to help reduce healthcare costs.”
The microfluidics system achieves both high multiplex and high throughput, and processes a range of sample types and volumes, ranging from 5 µL to 5 mL.
Rheonix has partnered with Life Technologies to use the microfluidics platform in the applied markets of food/beverage testing and animal health. The platform was selected based on cost, ease-of-use, and the ability to rapidly migrate existing benchtop assays to a fully automated system.

The EncompassMDx from Rheonix is a next-gen-eration molecular diagnostics platform incorp-orating multitarget “sample-to-answer” work-flow. The user loads samples and a consumable cartridge; sample manipulation and assay steps are contained within the system.
Next-Generation Sequencing
At Knight Diagnostic Laboratories, Ion Torrent™ technology is used for next-generation sequencing (NGS). This approach allows laboratory-developed tests (LDTs) to be performed that comprise oncology panels with 23–43 genes. The LDTs are focused on actionable mutations that are targetable with either FDA-approved drugs or therapeutics in clinical trials.
“We take a look at the tumor and then try to find a personalized cancer care option for patients who have failed standard of care. In addition to oncologists at our university, we serve a number of community practices around the country,” said Christopher L. Corless, M.D., Ph.D., surgical pathologist and CMO at Knight Diagnostic Laboratories, Oregon Health & Science University.
“A large pharmaceutical company told us if you can find us patients with mutations, then we will provide therapeutics. That started driving the testing. In the last four months we have performed tests on over 400 patients and identified treatment opportunities for a lot of them.”
The LDTs and potential observations are heavily biased toward experimental therapies. This means there is the chance that oncologists may not be able to get the needed therapeutic, or that it will not be reimbursed.
“It is a tough environment,” said Dr. Corless. “Labs like ours want to test more genes. So we are working to reduce the cost of NGS-based testing to the point where it is little more expensive than standard testing. Payers are technology agnostic, but if it is not standard of care, they want to see data that demonstrates the test is necessary. However, proving medical necessity is a slow process because we are trying to do this across many cancers at the same time.”
“A personalized approach does result in better care and better outcomes for many patients, but it is difficult to prove up front that broader-based testing is a good value proposition for all patients. That is why it is so important to further drive down the costs of NGS. In the future, NGS will allow us to become smarter on how to use and combine drugs and to understand what happens when a tumor becomes resistant to treatment,” added Dr. Corless.
NGS platforms are still relatively new technology and fairly labor intensive. Expertise is required to understand how the mutations should be interpreted and reported. As the technology matures and becomes easier to use, and as techniques are found for dealing with the vast amount of information generated, NGS will be implemented more broadly in the clinical setting.
Regulatory Issues
The sequencing of human genomes and the identification of associations between specific genetic variations and diseases will enable more precise therapeutic intervention, prediction of risk, and detection of residual disease.
“The area that is experiencing the highest acceleration is cancer genomics. NGS is providing tremendous opportunities for genomic-based diagnostic tests and for drug developers to better guide patient care. Gene-disease associations have the potential to revolutionize drug production [and to] accelerate and lower the cost of drug development,” stated Melina Cimler, Ph.D., vice president of quality and regulatory affairs at Illumina.
Gaining widespread acceptance of novel technologies in clinical applications is highly dependent on a number of key enablers. These include transparent and predictable risk-based regulatory pathways, reasonable evidence of clinical utility, and new economic models for reimbursement. The models should determine a test’s value not just by the cost of performing the test, but by the test’s ability to reduce use of ineffective therapies and improve clinical outcomes.
On the regulatory front, traditional pathways are too tortuous to allow rapid introduction of NGS into the clinical space. When a test involving NGS is evaluated by the FDA, it receives the same scrutiny as any other diagnostic test.
The FDA’s evaluation of safety and effectiveness is based on satisfactory analytical performance, clinical performance, compliance with labeling regulations for IVDs, and other factors, such as the ability to repeatedly manufacture the device to specifications. Clearly defining the intended use and indications for use helps determine the level of evidence expected.
NGS, which looks at the whole genome, or large elements of it, instead of just a few mutations in one gene, creates new challenges. The FDA understands the hurdles and is collaborating closely with a number of stakeholders to define pathways that ensure safety and effectiveness while encouraging innovation.
“NGS can interrogate the full complexity of genomes with customizable breadth and depth of coverage. Regulatory pathways will likely have to be very fluid for a few years, as the medical practice becomes more iterative and less population-based,” said Dr. Cimler. “Looking ahead, it is likely we will see more use of adaptive trial design. For clinical validation, building databases to increase generalizable knowledge linking genotypes and phenotypes will help provide needed evidence.”

Illumina’s MiSeqDx Cystic Fibrosis System has been submitted for FDA review. It consists of a next-generation sequencing instrument, two assays, and associated software.