January 1, 2017 (Vol. 37, No. 1)
NYU Professor Advances Autoimmune Disease Therapeutics
Jan Vilcek, M.D., Ph.D., is a professor of microbiology at New York University Langone Medicine Center. Research in his laboratory led to the development of cA2, the first chimeric monoclonal antibody against human tumor necrosis factor (TNF), which, when tested in human patients with rheumatoid arthritis (RA), led to the finding published in The Lancet in 1994 that “specific cytokine blockade can be effective in human inflammatory disease.” Successful clinical trials and evidence of the long-term safety of the monoclonal antibody led Centocor, later acquired by Johnson & Johnson, to commercialize Remicade, initially for the treatment of Crohn’s disease and eventually indicated for treating rheumatoid arthritis, ankylosing spondylitis, ulcerative colitis, and various other chronic inflammatory disorders.

Jan Vilcek, M.D., Ph.D., Professor of Microbiology, NYU Langone Medicine Center
GEN: How would you describe the impact of cA2 and Remicade on the area of autoimmune disease therapeutics? How did it change perceptions at the time and what role did it play in launching new classes of drugs and novel therapeutic approaches?
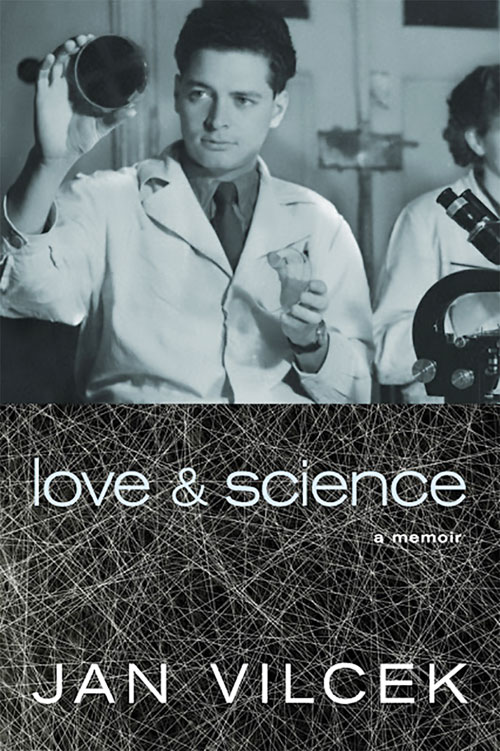
Dr. Vilcek: As you mention, the antibody that forms the core of Remicade was developed in my laboratory at NYU Medical Center. It was not a straightforward process and serendipity played a huge role. I describe the often unexpected twists and turns in the process of Remicade development in my recently published memoir, Love and Science.
Although it did not become apparent immediately after its approval by the FDA, the impact of Remicade on the clinical management of several autoimmune disorders has turned out to be profound. Let me use Crohn’s disease as an example. Before Remicade there was no really effective treatment for Crohn’s (prednisone, azathioprine, mesalazine, other anti-inflammatory agents were used). Now, with Remicade and other anti-TNF agents, the majority of Crohn’s patients can live normal lives. That is a huge change. These treatments also eliminate or greatly reduce the need for surgery, and they prevent intestinal cancer that occurs in untreated or inappropriately treated patients due to chronic inflammation.
RA is another disease in which anti-TNF therapy has played a huge role. Before anti-TNF therapy, RA was a debilitating disease, often leading to joint damage with major joint malformations, plus systemic disease that could lead to early death. With the help of anti-TNF, disease symptoms can largely be controlled and disease progression can be arrested or at least slowed.
cA2/Remicade was the first anti-TNF agent shown to be effective in RA and Crohn’s and, therefore, it had a huge impact on the development of other anti-TNF therapies and, ultimately, other anticytokine therapies. There are now many other approved anti-TNF agents available on the market, including some biosimilars. The development of these therapeutics would not have happened, or at least would have been substantially delayed, without the original demonstration of cA2’s activity in RA and Crohn’s.
Along the way, there were many surprises. No one expected that anti-TNF therapies would be effective in so many other autoimmune inflammatory disorders—ulcerative colitis, ankylosing spondylitis, psoriatic arthritis, plaque psoriasis, and the list goes on. And there are still new indications coming up for anti-TNF therapy; for example, hidradenitis suppurativa (HS, inflammatory subcutaneous lesions) can be treated with anti-TNF agents. The anti-TNF drug Humira was recently approved for HS by the FDA. Also, more evidence is upcoming in uveitis, as a Phase III trial with Humira is underway in uveitis.
GEN: In Love and Science: a Memoir (Seven Stories Press, New York, NY), you write, “For reasons that are still poorly understood, around 30–40% of patients with rheumatoid arthritis, Crohn’s disease, and the other conditions for which Remicade is approved do not respond adequately to these treatments. Unfortunately, it is still not possible to predict who will and who will not have a favorable response.” This is the case for many medications, and one of the driving forces behind the push toward personalized medicine. What progress is being made in this area and how is this problem being approached?
Dr. Vilcek: You are right, there is a great need for predictive tests that would enable a more personalized approach to the treatment of autoimmune diseases. There are still no reliable predictive tests available, but there may be some slow progress toward this goal.
In a recent publication, gene array studies in mucosal biopsies from patients with ulcerative colitis identified predictive panels of genes for (non-) response to infliximab. The study concluded that further study of the pathways involved should allow for a better understanding of the mechanisms of resistance to infliximab therapy in ulcerative colitis. Still, we have a long way to go.
I should add that it can be difficult to know how successful anti-TNF treatment is going to be, even after the initiation of therapy. A recent document issued by the NIH concluded: “There is no established and reliable non-invasive test that can predict whether a person with Crohn’s disease is responding to therapy early in the course of treatment when these evaluations may be inconclusive.” In such patients, it may be necessary to measure inflammatory markers or assess disease activity by analyzing intestinal biopsies.
It is easier to determine future therapeutic strategies if a patient initially responds to therapy and then stops responding. In such patients, it is possible to determine blood levels of the drug and, if they are inadequate, we can look for antibodies to the therapeutic antibody. If blood levels are inadequate, or if there are antibodies, it is possible to switch to another anti-TNF therapeutic or to another biologic therapy altogether (e.g., rituxan in RA).

Development of the drug now known as infliximab, or Remicade, began with the production of mouse antibodies, which needed to be modified to solve a basic problem—the human immune system doesn’t react well to mouse proteins. Selected mouse antibody domains were replaced with human antibody domains to create a chimeric mouse-human monoclonal antibody. The flowchart depicts the generation of the chimeric antibody, which neutralizes tumor necrosis factor (TNF) and is used for the treatment of Crohn’s disease, rheumatoid arthritis, and several other inflammatory disorders.
GEN: At present, no cures exist for autoimmune diseases. What types of advances are needed at the basic biology and/or applied research levels to be able to achieve a cure, and even identify early-stage pathology and intervene before clinical symptoms appear?
Dr. Vilcek: A cure is difficult, partly because we don’t understand the root cause of autoimmune diseases. I discuss this issue quite extensively in my book. Some people have expressed skepticism whether the pharmaceutical industry is at all interested in developing a cure, because that would cut into profits earned by making drugs that can keep the disease in check by having patients use them for the rest of their lives. Personally, I am less cynical; but I can see that developing cures will take much more time.
As to what might work as a cure, Dr. Marc Feldmann [professor at the University of Oxford], a pioneer in the development of anti-cytokine therapy of RA, believes that combination therapies might do the trick. He points out that anti-TNF therapy works better in combination with methotrexate than as monotherapy. He feels that it may take the extended use of a combination of three or four drugs, as is the case in patients infected with HIV or TB, to achieve a cure in autoimmune diseases. (Detractors might argue that even in HIV or TB, combination therapy does not lead to eradication of the infection.) Some combinations don’t work and might even be dangerous—e.g., anti-TNF plus anti-IL-1—because they suppress the immune system too strongly and greatly increase susceptibility to infections. But, perhaps anti-TNF with antibody to IL-17, which has a very different spectrum of actions than TNF, might work. Or perhaps anti-TNF with the blockade of metalloproteases in RA or some other combinations.
GEN: You write in your memoir, “The medical and commercial success of Remicade illustrates the value of university-based biomedical research for therapeutic advances and economic progress. (I hope policymakers in Washington will read these lines.)” Please discuss your perspectives on the effects of reduced government funding of academic biomedical research and the current trend that tends to emphasize applied and translational research at the expense of basic science. What is the risk of this trend for future new drug discovery—truly new treatment paradigms and not just “me-too” drugs?
Dr. Vilcek: The cuts in support for basic research spell disaster. There are many examples of innovative therapies (including the anti-TNF and other anti-cytokine therapies) that would not exist without the support of basic research. Let me quote from an interview given by Harold Varmus, the former director of the NIH (later president of the Memorial Sloan-Kettering Cancer Center and director of the National Cancer Institute):
“Just investing in clinical trials and things that are very disease-specific would be a huge mistake. Look at what pride people take now in advances made in diabetes and cancer research and infectious disease research. Almost all of it is based on recombinant DNA technology, genomics, and protein chemistry. These are methods that grew out of basic science that was funded for years and years in a noncategorical way.”
I feel strongly that without continued, generous support of basic research there soon will be nothing left to “translate.”
GEN: You detail the many and generous forms of philanthropy you and your wife have aspired to, and these have spanned the sciences. Why has it been so important to you to support both scientific research and art at such a high level?
Dr. Vilcek: As you said, my wife Marica’s background had a lot to do with the fact that our foundation combines the support of biomedical science with the backing of the arts and humanities. One common feature of science and the arts is that they both require a high degree of inventiveness, creativity, and originality.
I should add that there is another facet to the mission of the Vilcek Foundation, which is raising public awareness of the contributions made by immigrants to the United States, especially in the sciences and the arts. This latter role is highly topical in the present political climate, characterized by the anti-immigrant sentiment of a segment of the population. I believe that much of the success of this country, especially in science but also in the arts, is attributable to the contributions of immigrants to the U.S. For example, two out of three winners of the 2016 $250,000 Blavatnik National Awards for Young Scientists are foreign-born, and so are 13 of the 17 U.S. scientists selected to receive the highly selective 2016 $500,000 Simmons Investigatorships in math, science, and related fields.



