February 15, 2010 (Vol. 30, No. 4)
Review of Opportunities and Challenges in this Rapidly Expanding Field of Study
The ability to reprogram somatic cells to generate induced pluripotent stem (iPS) cells has generated tremendous interest and discussion since iPS cells were first produced from mouse cells in 2006 and human cells in 2007.
The reversion of differentiated cells to a state resembling embryonic stem cells offers a wealth of opportunities for disease researchers. Interest in iPS cells is expanding rapidly beyond the domain of stem cell experts to researchers modeling complex diseases in vitro and pursuing novel therapeutics.
“With iPS cell technology, you can now take a skin biopsy from a patient with a genetic disease such as familial Alzheimer or Lou Gehrig disease and turn their somatic cells into stem cells,” explains Chad Cowan, Ph.D., of the Harvard Stem Cell Institute. “You can then take those stem cells and turn them into cell types that might be affected in the disease.”
Along with the opportunities offered by iPS cells, practical challenges still abound. Culturing stem cells relies on both science and art and defining just what exactly constitutes a stem or iPS cell is stimulating a good deal of discussion.
Having standards for iPS cells could help define the differences between these murine embryonic stem cells and their induced counterparts.
Disease Modeling
Dr. Cowan’s lab is using iPS cells to support studies of obesity and metabolic disorders. While the lab can easily obtain fat cells from patients, these cells can’t be cultured over the long term. “We can keep the fat cells alive for a short period of time but that only allows us to do a one-time endpoint assay. It doesn’t allow us to tease out the complexities of what might be going wrong in a patient with a metabolic disorder. The ability to make patient-specific fat cells from iPS cells completely changes the game.”
With iPS cells, the lab can conduct dozens of assays to identify differences in fat cells from a person with a metabolic disorder such as type 2 diabetes versus a person with normal body weight or someone without diabetes. The ability to take a single genotype and potentially make any of the tissues that might be involved in a metabolic disorder such as hypothalamus, pancreatic beta cells, and hepatocytes, could lead to powerful disease models.
In his lab at the University of California, Santa Barbara, Dennis Clegg, Ph.D., is using iPS cells as one tool to study the loss of vision in age-related macular degeneration (AMD). In AMD, the degeneration of retinal pigment epithelial (RPE) cells appears to cause the death of neighboring rods and cones in the macular region of the central retina.
Dr. Clegg’s lab is evaluating the use of iPS-derived RPE cells to treat AMD and using iPS cell lines to create ocular cells, which can be used to study how the eye develops. “The real utility of iPS cells is that you can study human cells and processes in ways you couldn’t do before,” notes Dr. Clegg.
Culture Challenge
iPS cells, in particular those that are human-derived, can be challenging to culture especially for those researchers who haven’t previously worked with stem cells. The challenges they present are similar to those encountered when culturing human embryonic stem cells, including:
- the requirement for constant feeding;
- spontaneous differentiation during routine culture, which requires manual removal of colonies;
- low viability following a freeze-thaw cycle;
- difficulty in directing differentiation toward a specific lineage.
For researchers who haven’t previously cultured stem cells, I suggest first working with mouse-derived iPS cells. These cells tend to be more robust than human cells and conditions for successful culture are well defined. Many researchers first test their hypotheses using mouse iPS cells and then transition to a human model system.
The technology to create iPS cells is evolving rapidly. The first studies reporting the creation of iPS cells used retroviral vectors to integrate a set of DNA transcription factors directly into the somatic cell genome. Upon activation, these genes convert the cells from their adult, differentiated status to an embryonic-like state. This process required multiple retroviral vectors in order to insert four different viruses—each vector delivering one reprogramming gene into the somatic cells’ DNA.
Since these first studies were published, researchers have been seeking ways to reprogram somatic cells without using retroviral vectors and avoiding use of transcription factors such as c-Myc that are known oncogenes. Viral delivery of transcription factors can also disrupt normal gene expression when the vectors integrate into the genome. The high number of genomic integrations—15 to 20—that typically occur when multiple viruses are used for reprogramming poses a safety risk if the cells are to be used for therapeutic purposes.
Recently, Boston University scientists developed a highly efficient method for creating iPS cells from mouse fibroblasts using a single viral vector instead of the multiple viruses typically required for reprogramming. Four commonly used vectors are incorporated into a single lentiviral vector containing all four genes.
If iPS cells are to be used for therapeutic purposes, permanent integration of transcription factors into the genome becomes a problem. Alternative approaches to reprogramming include use of adenoviral delivery as the adenovirus does not integrate into the genome and transient transfection with transcription factors. Ultimately, it may be possible to use proteins or small molecules to direct the reprogramming process.
Standards, Anyone?
The rapid development and continued evolution of iPS technology has sparked discussions about the need for establishing standards to guide the field.
As researchers seek new methods to create iPS cells without genetic modification and the use of these cells to develop disease models continues to expand rapidly, questions arise as to whether these cells have the same properties and potential as embryonic stem cells. How can a researcher know for certain that he or she has generated iPS cells? Is there a minimum set of criteria for assessing whether a somatic cell is fully pluripotent or only partially reprogrammed?
Adding to this complexity, researchers also seek to understand the variation between iPS cell lines derived from a common somatic source.
Dr. Clegg’s lab is looking at the similarities and differences between iPS cell lines derived from human fetal RPE cells. “The question we were trying to address,” describes Dr. Clegg, “is if we take those cells down to iPS cells and just let them spontaneously differentiate, will they have some sort of epigenetic memory and tend to re-differentiate back into RPE or something else?
“The first line we looked at snapped back in large quantities to RPE cells,” reports Dr. Clegg. “But each subsequent line we looked at was different. That’s an important lesson for people to understand—each iPS line that’s generated is slightly different, just like each embryonic stem cell line is slightly different. They have different propensities for differentiation. They may have different epigenetics. They may have different expression patterns.”
“We’re still learning to define what is the best iPS cell,” notes Dr. Cowan. “The best function identically to an embryonic stem cell. It remains pluripotent, expands, and self-renews and it can differentiate into the types of tissues you’re interested in.”
An article by Maherali and Hochedlinger (Cell Stem Cell Protocol Review, December 4, 2008) suggests a minimal set of criteria that should be fulfilled in order to ascertain that a genuine iPS cell has been generated. The criteria include:
- all morphological attributes including unlimited self-renewal;
- expression of key pluripotency genes with downregulation of lineage-specific genes associated with the cell of origin;
- transgene independence;
- proof of functional differentiation through the highest stringency test acceptable.
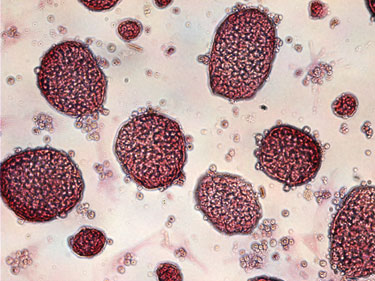
With human iPS cells, pluripotency can be assessed based on teratoma formation, which is a specific type of tumor containing cells from all three germ layers.
Researchers are also probing the similarity of iPS cell and embryonic cells through microarray studies, high-throughput sequencing, assessment of DNA methylation status at pluripotent cell specific genes, and by examining a range of protein biomarkers.
As our understanding of the similarities and differences between iPS cells and embryonic stem cells grows, new tools to identify and compare these cell types are needed. For example, live-cell imaging can be used to distinguish between human iPS cells and partially reprogrammed cells.
While standards provide a good basis of comparison, Dr. Cowan suggests that standards can be restrictive. “The standards are naturally evolving. We certainly need to maintain a minimum standard and recognize the standard will change over time. Within a year or two, there will probably be a new set of guidelines available. But there may be times when you may not want to make something that is an embryonic cell.
“In fact, it may be more to your advantage to somehow uniquely trap a cell so that it is lineage-committed to something that can replicate in culture indefinitely but really only thinks of itself as ‘lung,’ for example, and so would only ever differentiate back to lung cell types.”
While a great deal remains to be learned about iPS cells, they represent a powerful new research tool. In addition to their potential impact on the field of regenerative medicine, use of iPS cells to dissect complicated diseases at the cellular level will provide valuable new insights supporting drug discovery. As we learn more about the nature of iPS cells, standards will certainly evolve and new tools will become available to facilitate efficient creation and routine culture.
Vi Chu, Ph.D. ([email protected]), is R&D manager, stem cell/cell biology at Millipore.



