The Influence of New Anti-HCV Therapy on the DNA Base Excision Repair System of Peripheral Blood Mononuclear Cells
Evidence suggests that the hepatitis C virus (HCV) can not only infect hepatocytes, but also other extrahepatic tissues (De Vita et al., 1995; Karavattathayyil et al., 2000; Akbayir et al., 2004; Simula et al., 2007). Kondo et al. (2011) suggest that the presence of the CD81 protein is crucial for virus propagation, as HCV can also infect lymphoid cells. Chronic hepatitis C can also lead to malignant lymphoma (De Vita et al., 1995). Several groups have suggested that lymphocytes might serve as a reservoir for HCV (Kondo and Shimosegawa, 2013), which is consistent with the fact that HCV therapy is complicated by the interaction between lymphoid cells and the virus, leading to a recurrence of the disease in a state that is difficult to treat. Moreover, Mizuochi et al. (2011) have shown that the CD27+ B cells are more susceptible to apoptosis when infected with HCV. It was also revealed that NS3/4A (nonstructural protein 3 and 4A) of HCV can interact with ATM (ataxia-telangiectasia mutated), a main protein kinase involved in DNA damage response (DDR) (Lai et al., 2008). In NS3/4A-expressing cells, dephosphorylation of phosphorylated ATM and γH2AX—a phosphorylated version of H2AX creating foci at DNA double-strand break (DSB) site—was delayed following exposure to ionizing radiation. This increased DNA damage, as shown by comet assay, and sensitized the cells to irradiation. Another study showed that peripheral blood mononuclear cells (PBMCs) of HCV-infected patients exhibited frequent chromosomal aberration and that in vitro infection of B cells caused increase of chromosomal breaks and sister chromatid exchanges (Machida et al., 2010). Furthermore, in those cells core protein of the virus interacted with NBS1 protein inhibiting formation of Mre11/RAD50/NBS1 (MRN) complex. MRN is crucial in both homologous recombination repair (HRR) and nonhomologous end joining (NHEJ). Disruption of this complex creation affected ATM activation and binding of other repair proteins to DSB. This resulted in hypersensitization of the cells to ionizing radiation and bleomycin, which both induce DSB. Latest studies showed that NS3/4A downregulated activity of CHK2 (checkpoint kinase 2) in B cells (Dai et al., 2016). This protein has a key role in DDR, since it stimulates expression of DNA repair proteins. Finally, comparison between high viral load and low viral load human hepatoma Huh-7.5.1 cells showed that the former cells exhibited greater amount of DNA strand breaks, as shown by γ-H2AX foci and comet assay, as well as lower expression of MRE11, phospho-ATM, and OGG1 (oxoguanine glycosylase) when compared with the former cells (Wang et al., 2017). Interestingly, OGG1 is involved in base excision repair (BER) pathway. Therefore, it is possible that the virus can affect efficacy of different DNA damage repair pathways of hepatocytes as well as PBMC. The present examines the effectiveness of the BER proteins in nuclear and mitochondrial extracts (NE and ME, respectively) of PBMC isolated from HCV-positive patients before and after therapy. The obtained results are then compared with a control (HCV-negative) trial group.
* Abstract
Hepatitis C virus (HCV) can infect extrahepatic tissues, including lymphocytes, creating reservoir of the virus. Moreover, HCV proteins can interact with DNA damage response proteins of infected cells. In this article we investigated the influence of the virus infection and a new ombitasvir/paritaprevir/ritonavir ± dasabuvir ± ribavirin (OBV/PTV/r ± DSV ± RBV) anti-HCV therapy on the PBMCs (peripheral blood mononuclear cells, mainly lymphocytes) DNA base excision repair (BER) system. BER protein activity was analyzed in the nuclear and mitochondrial extracts (NE and ME) of PBMC isolated from patients before and after therapy, and from subjects without HCV, using modeled double-strand DNA, with 2′-deoxyuridine substitution as the DNA damage. The NE and ME obtained from patients before therapy demonstrated lower efficacy of 2′-deoxyuridine removal and DNA repair polymerization than those of the control group or patients after therapy. Moreover, the extracts from the patients after therapy had similar activity to those from the control group. However, the efficacy of apurinic/apyrimidinic site excision in NE did not differ between the studied groups. We postulate that infection of lymphocytes by the HCV can lead to a decrease in the activity of BER enzymes. However, the use of novel therapy results in the improvement of glycosylase activity as well as the regeneration of endonuclease and other crucial repair enzymes.
Discussion
The most frequent DNA lesions (8-oxoguanine, thymine glycol, dihydrothymine, dU) (De Bont and van Larebeke, 2014) are removed from the genome by the BER (Kim and Wilson, 2012) (Figure 1). This repair system is initiated by specific glycosylases leading to short (SP) or long patch (LP) subpathways, which are differentiated by polymerase activity: in the SP, only one nucleotide is replaced by the correct one, whereas in the LP, two or more nucleotides are incorporated. Glycosylases play a crucial role in BER, as they initiate the pathway by recognizing and excising specifically modified bases. If these enzymes are lacking or fail to function properly, the DNA damage can be camouflaged to the p53 protein, thus preventing the apoptosis process from being triggered and prolonging the cell lifespan (Lakin and Jackson, 1999; Meek, 2004; Culmsee and Mattson, 2005). Since HCV can infect B lymphocytes and prolong their lifespan, the present study investigates the activity of selected BER proteins (UDG, APEX1, and polymerases) in NE and ME of PBMC.
Figure 1.
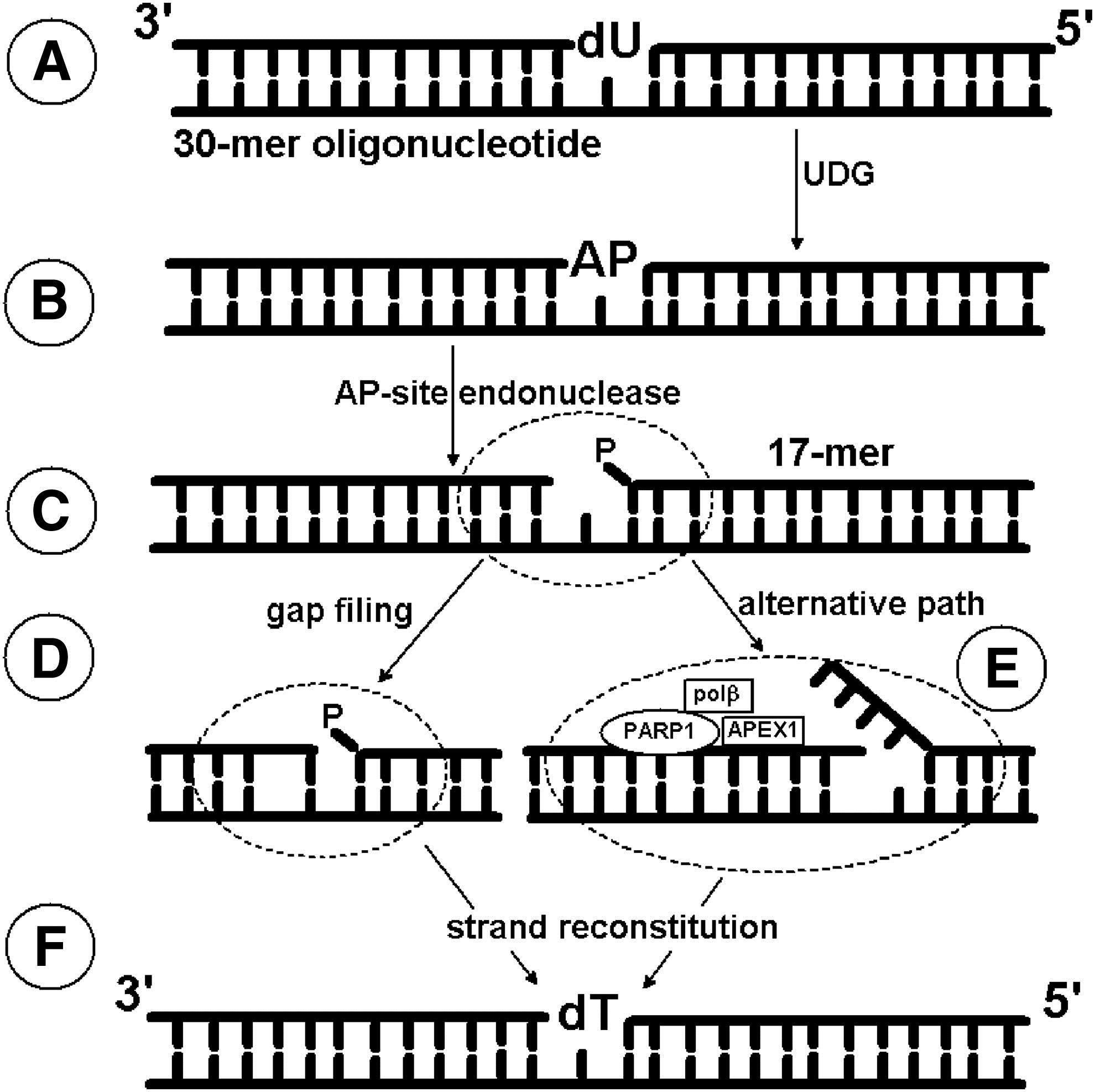
In our study, we used a modeled 30-mer double-strand oligonucleotide containing 2′-deoxyuridine (dU) as a DNA lesion. dU can appear in the genome due to cytidine deaminase activity, spontaneous 2′-deoxycytidine deamination, misincorporation instead of thymidine during replication, leading to an A:U mismatch formation. Consequently, the presence of dU as a DNA lesion is highly mutagenic and can be lethal to a cell. All organisms possess the following enzymes: uracil-DNA glycosylase removing dU from the genome and dUTP pyrophosphatase hydrolyzing 2′-deoxyuridine-5′-triphosphate (the substrate for polymerase) (Ingraham et al., 1986; Impellizzeri et al., 1991; Vassylyev and Morikawa, 1996; Vasilenko and Nevinsky, 2003). Therefore, we examined the effectiveness of the glycosylytic activity in NE and ME.
Click to read the entire article and its references.
DNA and Cell Biology, published by Mary Ann Liebert, Inc., is the trusted source for authoritative, peer-reviewed reporting on the latest research in the field of molecular biology. The above article was first published in the July 2017 issue of DNA and Cell Biology with the title “The Influence of Hepatitis C Virus Therapy on the DNA Base Excision Repair System of Peripheral Blood Mononuclear Cells". The views expressed here are those of the authors and are not necessarily those of DNA and Cell Biology, Mary Ann Liebert, Inc., publishers, or their affiliates. No endorsement of any entity or technology is implied.