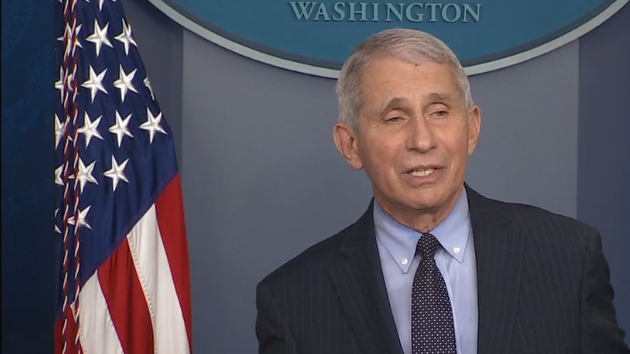
Viral Immunology Journal’s editor-in-chief Dr. Rod Russell from Memorial University of Newfoundland and Labrador, had the distinct pleasure to speak Dr. Anthony Fauci.
Anthony S. Fauci, MD, is director of the National Institute of Allergy and Infectious Diseases (NIAID) at the U.S. National Institutes of Health, where he oversees an extensive research portfolio devoted to preventing, diagnosing, and treating infectious and immune-mediated diseases. Dr. Fauci has been a key advisor to seven Presidents and their administrations on global HIV/AIDS issues, and on initiatives to bolster medical and public health preparedness against emerging infectious disease threats such as pandemic influenza and COVID-19. Currently, he is the Chief Medical Advisor to President Joe Biden. As an HIV/AIDS researcher he has been involved in the scientific effort since AIDS was recognized in 1981, conducting pivotal studies that underpin the current understanding of the disease and efforts to develop therapies and tools of prevention. Dr. Fauci was one of the principal architects of the President’s Emergency Plan for AIDS Relief (PEPFAR), which has helped save millions of lives throughout the developing world and for which he has received the Presidential Medal of Freedom (the highest honor given to a civilian by the President of the United States). Other awards include the National Medal of Science and the Mary Woodard Lasker Award for Public Service.
Viral Immunology: We know you are a very busy man, so let us get right into the discussion. I wanted to talk today about three themes. We can talk a little about the pandemic and your thoughts on that, as well as some reflection on HIV/AIDS and the work you have done over your career, and some general career points that you might want to share. Let’s jump right in. How do you feel the pandemic has affected vaccine literacy in North America and globally?
Dr. Fauci: It’s interesting because it depends on what people mean by vaccine literacy. If you mean the awareness of the importance of vaccines, I think it is heightened in some respects greatly; the appreciation by people of the life-saving aspects of vaccines has increased. If anyone seriously looks at the data of the degree and level of hospitalizations, serious disease, often leading to death in the unvaccinated versus the vaccinated, the data are as striking as you could imagine. The overwhelming majority of people, regardless of their underlying status that go on to severe disease leading to hospitalizations and death, are either among the unvaccinated or those who have been vaccinated but not kept up-to-date on their boosting.
In contrast, we are in an era, unfortunately, of antiscience, which is part of antivax, which is a very frustrating situation whereby you have a historic pandemic, which in the United States alone has led to the loss of over 1 million lives and incontrovertible proof that vaccines save millions of lives. And yet, there are so many people in the United States and throughout the world who refuse to get vaccinated because of a fundamental core antivax attitude that is related in many respects to anything from pure disinformation to political ideology, which is really quite frustrating when you are dealing with a public health challenge.
Viral Immunology: Yes, I agree, for sure. What would you say was the most unexpected aspect of the pandemic, in your opinion? I guess I would mean with respect to the virus itself and the curve balls that it threw us, as well as in regard to the public’s response to the pandemic.
Dr. Fauci: Why don’t we take one of those at a time? The most unexpected aspect of the pandemic from both the virus itself and the epidemiology is the unprecedented nature of the emergence of new variants in a manner that leads to a drifting or changing of the virus approximately every 4 or so months, not only in the United States, but also in Canada and throughout the world. If you look at the evolution of this outbreak, we have never really seen anything even approaching what we are now experiencing. We have drifting of influenza virus from year to year, but we do not have the extent of variant emergence that we have seen with SARS-CoV-2.
The other unexpected element of this was the very short durability of protection from prior infection or prior vaccination. When you get infected with or vaccinated against viruses such as polio, measles, and smallpox, the durability of protection is measured in decades at worst and over a lifetime at best. And yet, with SARS-CoV-2, the durability of protection is really strikingly short.
The public response to the pandemic is what I mentioned just a bit ago, which is the extraordinary phenomenon of the availability of life-savings vaccines, and the fact that, for example, in the United States, only 68% of the population is vaccinated and only about one half of those have been boosted, which seems almost inexplicable that that is happening, but it is.
Viral Immunology: If we can stay there for a moment, with the short duration of protection with the vaccines, and after natural infection, what do you think we are going to need going forward? Are we going to need a better vaccine? Do you think that will give us longer protection or is this just what happens with coronaviruses and we are never going to see a longer duration of protection?
Dr. Fauci: Well, I think there are two or three aspects of what is going to be needed regarding the relationship between vaccines and durability and depth and breadth of protection. We have great vaccines. I mean, some of the great scientific breakthroughs of the last few years have been the mRNA vaccine and immunogen design based on structure-based vaccine design. But even with that advance, we do need better vaccine platforms and immunogens to lead to greater durability and breadth of protection. That could be nanoparticles, or that could be vector-based expression of immunogens.
Also, we are going to need better protection against infection and transmission for a number of reasons, because we now know that the vaccines that we have, although they still do a very good job of protecting you against severe disease, when we look at protection against infection, how many people do we all know, myself included, that were vaccinated, doubly boosted, and still got infected. The protection against severity of disease is pretty good, but if you really want to suppress the virus by suppressing acquisition as well as transmission, we have got to have better vaccines.
Viral Immunology: So, Dr. Fauci, that’s an interesting perspective for sure. Let us switch gears now and talk a little about HIV/AIDS, which has been the focus of much of your career. The late Mark Wainberg, who I know you knew well, told me once that you said you hoped to see one person cured of HIV in your lifetime, and now we have seen that. What do you hope we might see in the next 50 years in the world of HIV/AIDS?
Dr. Fauci: Well, we have got to be careful when discussing the person, or few persons, who have been cured of HIV in the sense of not requiring daily medication and yet having the virus be completely absent from their body, essentially having the virus eradicated from their bodies. That has only happened in very unusual circumstances of stem cell transplantation, with the very aggressive conditioning that’s associated with that, in people who have an underlying condition such as a lymphoma or a leukemia that required a stem cell transplantation to begin with.
Although that is a proof of concept, it is not a practical approach to the idea of curing people. However, what we have done extremely successfully is develop an array of drugs in combination, sometimes contained in one pill, that can chronically and durably suppress the virus to below detectable level. This not only saves the life of individuals who are being treated and essentially allows them to have an essentially normal lifespan, but it also makes it virtually impossible for them to transmit the virus to someone else.
The terminology of undetectable equals untransmittable [U = U]. That is a major advance. What we have done now over the last few years is to make the therapeutic approach much easier and user friendly, such as with long-acting injectable drugs, which can be given every couple of months. I believe as we get better at it over the coming months and years, it may be that you can give an injectable drug maybe twice a year and continue to suppress the virus below detectable level. That is not a classical cure in the sense of eradication, which we will continue to try to do, but the advances that have been made in therapy now are really quite breathtaking in their success.
The above article has been edited for length. To read the original Dr. Anthony Fauci Reflects on His 54-Year Career at NIH visit Viral Immunology. Viral Immunology, from GEN‘s parent company Mary Ann Liebert, Inc., delivers cutting-edge peer-reviewed research on rare, emerging, and under-studied viruses, with special focus on analyzing mutual relationships between external viruses and internal immunity. Original research, reviews, and commentaries on relevant viruses are presented in clinical, translational, and basic science articles for researchers in multiple disciplines.