After decades in which no novel therapeutic treatments were approved for acute myeloid leukemia (AML), the past few years have seen the approval of several groundbreaking therapies for the disease.1 One of the most rapidly adopted agents is venetoclax (ABT-199), which results in favorable response rates and improved overall survival when used in combination with hypomethylating agents or low-dose cytarabine. Venetoclax exerts its antitumor effects through inhibition of the antiapoptotic protein B-cell lymphoma-2 (Bcl-2), thereby restoring the cellular process of apoptosis.2,3
Unfortunately, as with all current therapies for AML, most patients treated with venetoclax will eventually relapse due to development of resistance mechanisms. For venetoclax, one resistance mechanism that may occur in tumor cells is the upregulation of other antiapoptotic pathway members such as myeloid cell leukemia-1 (Mcl-1) protein, thereby circumventing the inhibitory effect of venetoclax on Bcl-2.4–8 To overcome the development of resistance, rational combinations that target distinct antiapoptotic pathway members and can potentially lead to synergy have become an area of burgeoning translational research.
Combatting resistance to venetoclax
Hematological cancers are radiation sensitive. An example of this phenomenon is highly relevant to AML patients for whom venetoclax treatment has failed. Specifically, radiation-mediated DNA damage is known to result in a decrease in Mcl-1 protein levels.9,10 Delivery of therapeutic levels of total body irradiation via external beam, however, is difficult to implement in hematological malignancies such as AML without significant toxicity.
Alternatively, targeted delivery of radiation can be achieved by antibody radionuclide conjugates (ARCs), where an antibody is linked to a radioactive isotope such as iodine-131 (131I) or actinium-225 (225Ac). ARCs are therefore a potentially more effective and better tolerated alternative to target and deliver high amounts of radiation directly to cancer cells.
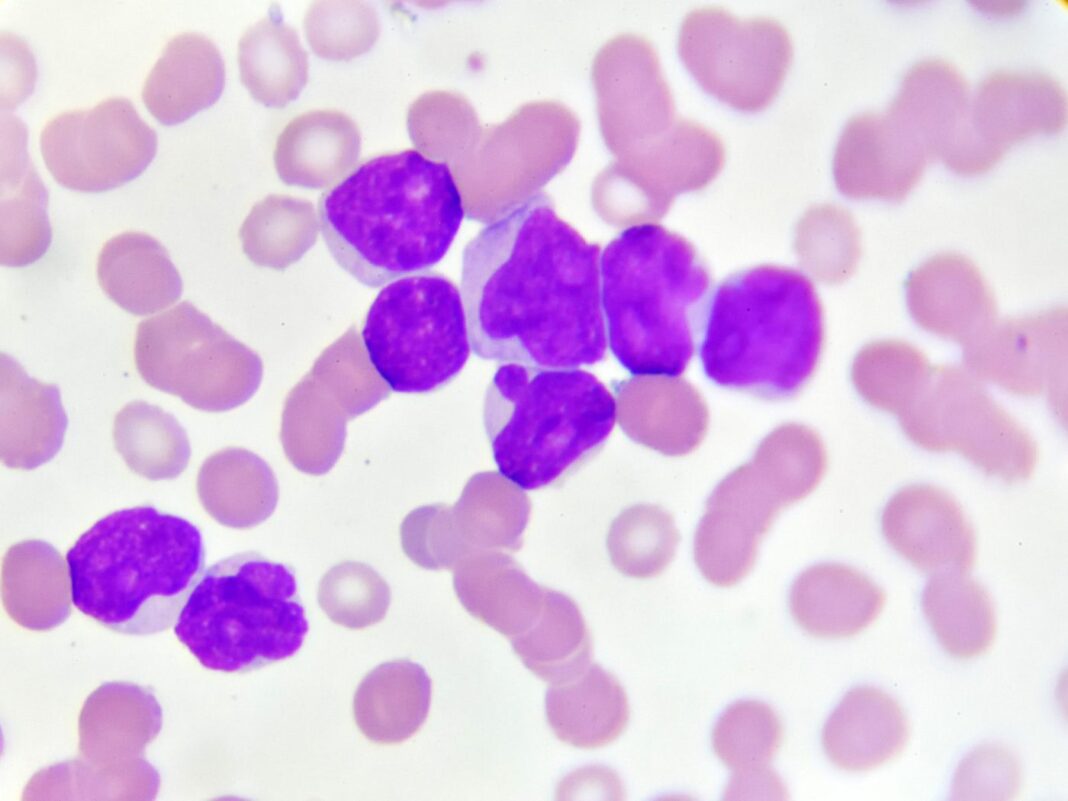
There have been several FDA-approved radioimmunoconjugate therapies, including Bexxar, Lutathera, and Azedra, and development of new ARCs is an active area of investigation in the biotechnology and pharmaceutical industries. Actinium Pharmaceuticals, a biotechnology company specializing in ARCs, has performed translational work investigating the use of ARCs to deliver targeted radiation to AML cells that, in addition to delivering potent single-agent tumor-cell-killing activity, may resensitize cells to venetoclax treatment when used in combination with venetoclax (Figure 1).

Preclinical results supporting the ARC–venetoclax combination strategy
CD33 is a validated therapeutic target for AML that is expressed on the majority of leukemic blasts and is not expressed outside of the immune system. Lintuzumab is an anti-CD33 monoclonal antibody that has been clinically evaluated as a naked antibody in multiple clinical trials, although a lack of efficacy led to its discontinuation in clinical trials.11–13 Given the favorable safety profile of lintuzumab, the antibody was pursued as an ARC.
225Ac-labeled radioimmunoconjugate lintuzumab (225Ac-lintuzumab, also known as Actimab-A) is currently being evaluated as a therapeutic for hematologic malignancies including AML and has demonstrated promising results as a single agent.14 Following the completion of single-agent Phase I and Phase II studies, the company has focused clinical development of 225Ac-lintuzumab in mechanism-based clinical combinations. To this end, low doses of 225Ac-lintuzumab are being evaluated in combination with the chemotherapy regimen CLAG-M.
Interim results reported in December 2019 demonstrated an 86% overall response rate with 71% of treated patients confirmed to have minimal residual disease (MRD)-negative status.15 These data lend further support to the idea that a combination of low doses of an ARC with other AML agents may lead to improved outcomes.
As an alpha-emitter, 225Ac emits four alpha particles that each have the potential to cause lethal DNA double-strand breaks. Given the link between DNA damage and decreases in levels of Mcl-1, it was hypothesized that a combination of venetoclax and 225Ac-lintuzumab may reverse resistance in AML cells that do not respond to venetoclax (Figure 1).
To evaluate the effect of a combination of venetoclax and 225Ac-lintuzumab on cell viability in cell lines, AML cells (OCI-AML3) that were known to be resistant to venetoclax were utilized. When IC50 doses of 225Ac-lintuzumab and of venetoclax were tested on the OCI-AML3 cells in culture, the combination of the two agents exhibited a 78% decrease in cell viability, statistically greater than the modest effects of each single agent.16 Western blotting for Mcl-1 in OCI-AML3 cells treated with 225Ac-lintuzumab revealed that levels were markedly decreased following exposure to the ARC, but not when treated with unlabeled lintuzumab.16
Given the promising in vitro data, the combination of 225Ac-lintuzumab and venetoclax was then tested in an animal model of AML using the venetoclax-resistant line OCI-AML3. Venetoclax was administered daily for 21 days, a regimen designed to mimic the clinical therapeutic dosing in AML patients. 225Ac-lintuzumab was given on day 1 alone, or on day 1 followed by the 21 days of venetoclax in the combination treatment group.
Single-agent venetoclax had no impact on tumor growth control, and all mice died by day 28. While 225Ac-lintuzumab as a single agent resulted in a significant control of tumor growth, combination treatment with venetoclax and 225Ac-lintuzumab was superior in terms of survival and tumor growth control and regression. The combination therapy was well tolerated, as indicated by minimal change in body weight in treated mice at the completion of the study.16
Conclusions
In summary, these promising preclinical data support the hypothesis that exposure of venetoclax-resistant AML cells to radiation delivered by a CD33-targeted ARC may resensitize cells to venetoclax and improve outcomes for AML patients. These data underpin the recently initiated clinical trial using 225Ac-lintuzumab in combination with venetoclax in relapsed-refractory AML patients.
The trial is being performed in collaboration with Gary J. Schiller, MD, at the University of California, Los Angeles. Similar to the combination trial of 225Ac-lintuzumab and CLAG-M, the Phase I portion of the trial, a dose escalation of 225Ac-lintuzumab, will be performed to determine the maximum tolerated dose of 225Ac-lintuzumab in combination with venetoclax, followed by a Phase II trial to measure overall response rates.
Dale L. Ludwig, PhD, is chief scientific officer and Eileen M. Geoghegan, PhD, is strategic research and business development manager at Actinium Pharmaceuticals.
References
1. Lai C, Doucette K, Norsworthy K. Recent drug approvals for acute myeloid leukemia. J. Hematol. Oncol. 2019; 12(1): 100. Published 2019 Sep 18. doi:10.1186/s13045-019-0774-x
2. DiNardo CD, Pratz K, Pullarkat V, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 2019; 133(1): 7–17.
3. Wei AH, Jr SAS, Hou J-Z, et al. Venetoclax Combined With Low-Dose Cytarabine for Previously Untreated Patients With Acute Myeloid Leukemia: Results From a Phase Ib/II Study. J. Clin. Oncol. 2019; 37(15): 1277–1284.
4. Niu X, Zhao J, Ma J, et al. Binding of Released Bim to Mcl-1 is a Mechanism of Intrinsic Resistance to ABT-199 which can be Overcome by Combination with Daunorubicin or Cytarabine in AML Cells. Clin. Cancer Res. 2016; 22(17): 4440–4451.
5. Tahir SK, Smith ML, Hessler P, et al. Potential mechanisms of resistance to venetoclax and strategies to circumvent it. BMC Cancer 2017; 17(1): 399.
6. Luedtke DA, Niu X, Pan Y, et al. Inhibition of Mcl-1 enhances cell death induced by the Bcl-2-selective inhibitor ABT-199 in acute myeloid leukemia cells. Signal Transduct. Target Ther. 2017; 2: 17012.
7. Punnoose EA, Leverson JD, Peale F, et al. Expression Profile of BCL-2, BCL-XL, and MCL-1 Predicts Pharmacological Response to the BCL-2 Selective Antagonist Venetoclax in Multiple Myeloma Models. Mol Cancer Ther. 2016; 15(5): 1132–1144.
8. Leverson JD, Cojocari D. Hematologic Tumor Cell Resistance to the BCL-2 Inhibitor Venetoclax: A Product of Its Microenvironment? Front. Oncol. 2018; 8: 458.
9. Wu H, Schiff DS, Lin Y, et al Ionizing radiation sensitizes breast cancer cells to Bcl-2 inhibitor, ABT-737, through regulating Mcl-1. Radiat. Res. 2014; 182(6): 618–625.
10. Nijhawan D, Fang M, Traer E, et al. Elimination of Mcl-1 is required for the initiation of apoptosis following ultraviolet irradiation. Genes Dev. 2003; 17(12): 1475–1486.
11. Feldman E, Kalaycio M, Weiner G, et al. Treatment of relapsed or refractory acute myeloid leukemia with humanized anti-CD33 monoclonal antibody HuM195. Leukemia 2003; 17(2): 314–318. doi: 10.1038/sj.leu.2402803
12. Feldman EJ, Brandwein J, Stone R, et al. Phase III randomized multicenter study of a humanized anti-CD33 monoclonal antibody, lintuzumab, in combination with chemotherapy, versus chemotherapy alone in patients with refractory or first-relapsed acute myeloid leukemia. J. Clin. Oncol. 2005; 23(18): 4110–4116. doi: 10.1200/JCO.2005.09.133
13. Sekeres MA, Lancet JE, Wood BL, et al. Randomized phase IIb study of low-dose cytarabine and lintuzumab versus low-dose cytarabine and placebo in older adults with untreated acute myeloid leukemia. Haematologica 2013;98(1):119–128. doi: 10.3324/haematol.2012.066613
14. Ehab L. Atallah, Johnnie J. Orozco, Michael Craig, Moshe Yair Levy, Laura E. Finn, Sharif S. Khan, Alexander E. Perl, Jae H. Park, Gail J. Roboz, William Tse, Kebede H. Begna, Raya Mawad, David A. Rizzieri, Mark S. Berger, Joseph G. Jurcic; A Phase 2 Study of Actinium-225 (225Ac)-Lintuzumab in Older Patients with Untreated Acute Myeloid Leukemia (AML) – Interim Analysis of 1.5 µci/Kg/Dose. Blood 2018; 132 (Supplement 1): 1457. doi: https://doi.org/10.1182/blood-2018-99-111951
15. Sameem Abedin, Guru Subramanian Guru Murthy, Lyndsey Runaas, Laura C. Michaelis, Ehab L. Atallah, Mehdi Hamadani, Alexandra M. Harrington, Karen Carlson; Lintuzumab Ac-225 in Combination with CLAG-M Chemotherapy in Relapsed/Refractory AML: Interim Results of a Phase I Study. Blood 2019; 134 (Suppl. 1): 2605. doi: https://doi.org/10.1182/blood-2019-122487
16. Ravendra Garg, Eileen Geoghegan, Kevin A. Allen, Wojciech Dawicki, Ekaterina Dadachova and Dale L. Ludwig Cancer Res. July 1 2019 (79) (13 Suppl.) 3808; doi: 10.1158/1538-7445.AM2019-3808