When you strike at a king, you must kill him. Otherwise, you’ll be vulnerable to the king’s counterstrike, which may be devastating. This warning is particularly apt if you intend to bring down King Cancer—or the Emperor of All Maladies, as he’s been called. King Cancer’s favorite counterstrikes include disabling the immune system and stirring up resistance to once-potent therapies.
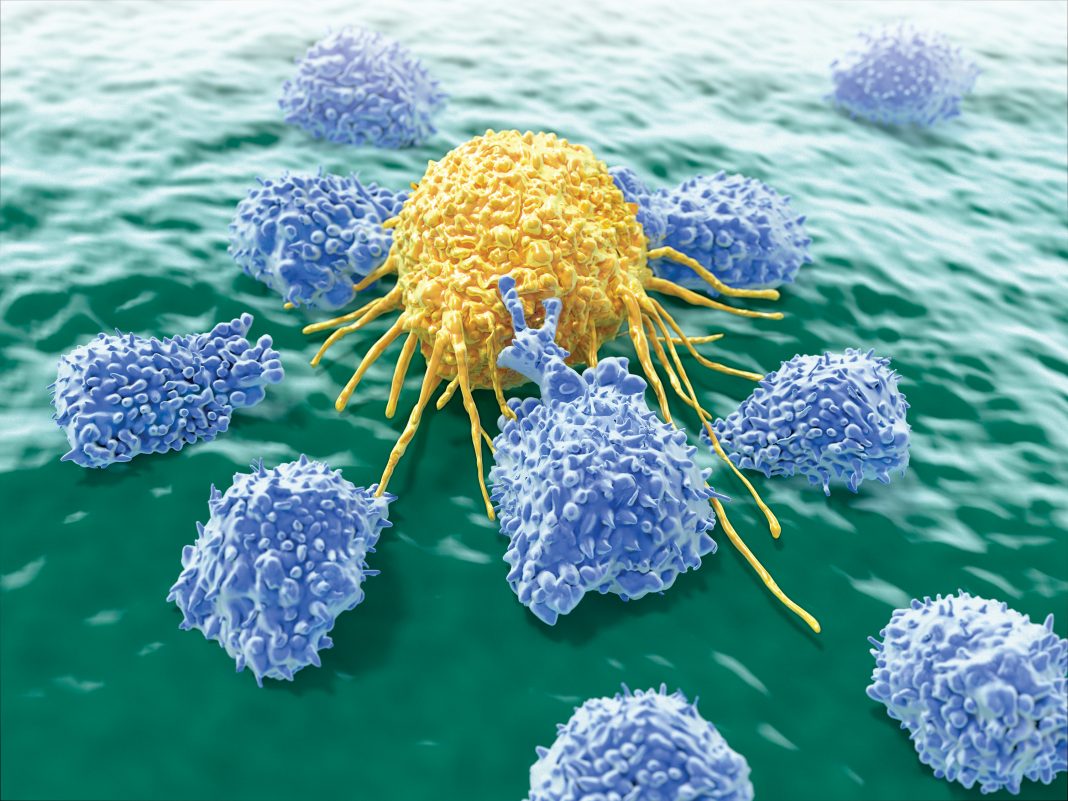
So, what does it take to put cancer down and, most important, keep it down? A coalition. According to the four scientists consulted in this article, the ultimate coalition is one that combines immune system elements and human-made factors. This coalition is called … cancer immunotherapy.
The four scientists offering their views on cancer immunotherapy are:
- Tibor Keler, PhD, Co-founder, Senior Vice President, and CSO, Celldex Therapeutics
- Sebastian Kreiter, MD, Senior Vice President and Head of Immunotherapy and Preclinical Research, BioNTech
- Lance Leopold, MD, Group Vice President, Clinical Development, Incyte
- Flavius Martin, MD, Vice President, Oncology and Inflammation Discovery Research, Amgen
These scientists suggest that if cancer immunotherapy is to succeed, it must achieve a delicate balance. Cancer immunotherapy should be broad enough to block the many paths of escape to which cancer may resort; at the same time, it should be targeted, hitting the right targets and, ideally, nothing else.
Finding the right balance is a key consideration in cancer immunotherapy approaches such as combination therapies and precision medicine. But before we delve into those topics, let’s address a preliminary point: the need to recognize and empower potential allies.
Sources of resistance
Observations of the immunity phenomenon go back to ancient Greece. In 430 BC, the historian named Thucydides noted that plague survivors acquired some sort of resistance to the disease. This intelligence, however, didn’t prove actionable.
Subsequent developments were more encouraging. For example, in the 1722, something like the first immunotherapy trial was managed by Scottish physician Charles Maitland. This trial, which included six inmates from Newgate Prison, tested the efficacy of an early form of smallpox vaccination. All the inmates survived. All were pardoned. A safer form of vaccination—from cowpox, not smallpox—was tested for the first time in 1796 when Edward Jenner inoculated young James Phipps.
Eventually, vaccination became widely recognized as a potent weapon against infectious disease. Then, in the late 19th century, a thought occurred to a physician named William B. Coley, MD. If vaccination primed the body against infectious disease, he reasoned, maybe it would work against cancer, too. He administered vaccines, his Coley Toxins, to hundreds of cancer patients. The results were mixed, at best. Still, Coley has come to be known as the “Father of Immunotherapy.”
Alas, in Coley’s time, immunity was still poorly understood, and antibiotics didn’t exist. So, medicine avoided cancer immunotherapy and worked on other approaches, namely, surgery, radiotherapy, and chemotherapy. In recent years, however, cancer immunotherapy started getting a second look, partly because the immune system was better understood. Another crucial development was the rise of genomics.
In the late 1990s to early 2000s, the first complete human genomes were sequenced, albeit painstakingly and expensively. Since then, improvements in sequencing have made it possible to study genetic variability in large human populations. Detailed knowledge of person-to-person variability provided clues to cancer risk and pathogenesis.
Even more potentially useful information came from the rise of transcriptomics, particularly single-cell sequencing, which can uncover cell-to-cell variability in an individual’s tissues.
“[Progressing] from population-level to single-cell analysis provides the ability to ‘zoom in’ on specific cells,” states Martin. “The explosion of data from single-cell omics, primarily driven by RNA sequencing, will one day map the full human body map at the single-cell level, in the healthy and the diseased. Integrating this baseline information with genetics and biological knowledge will allow focus on the immune pathways for target prioritization and the development of the next generation of hypotheses.”
In addition, a deeper understanding of the complex interplay of cells in the tumor microenvironment will lead to therapies directed at the specific mechanism of immune suppression in a specific patient. “This precise approach, says Leopold, “may improve our ability to predict and improve outcomes.”
Checkpoint inhibition and combination therapy
Two decades ago, when genomic sequencing was just getting started, doubts lingered over the ability of the immune system to mount potent antitumor immunity. Since then, not only has sequencing become more sophisticated, medical science has improved its understanding of the immune system’s role in controlling cancer. In particular, scientists have discovered the power of immune checkpoint inhibitors. These are drugs that bind to checkpoint proteins, which are signaling proteins that occur on the surface of tumor cells and T cells. By binding to checkpoints, the drugs can turn an “off” signal “on,” prompting T cells to attack cancer cells.
Pioneering work on checkpoint inhibitors was conducted in the 1990s by James P. Allison and Tasuku Honjo. Allison studied the T-cell protein CTLA-4, and Tasuku studied another T-cell protein, PD-1. Both proteins, they determined, function as T-cell brakes. They also demonstrated strategies for inhibiting these brakes in the treatment of cancer. This work, which was recognized with a Noble Prize in 2018, inspired drug developers.
“The dramatic impact of checkpoint inhibitors in many cancer patients has brought immunotherapy to the forefront of cancer treatment,” declares Keler. “[It has] fundamentally changing the mindset of drug development companies.”
Researchers noticed how cancer immunotherapy, compared to chemotherapy, improved overall survival and progression-free survival in cancer patients, as quantified with Kaplan-Meier curves.
The first checkpoint inhibitor (CPI) was approved by the FDA in 2011. Called ipilimumab, this CPI is a CTLA-4 inhibitor. It was shown to extend overall survival in patients with advanced melanoma, and it is now used to treat multiple cancers. PD-L1 inhibitors followed. They are changing the prognosis of many difficult-to-treat cancers, notes Leopold.
After initial success as monotherapies, CPIs are now being increasingly used in combination therapies. Several of these have shown even better long-term outcomes. Many trials testing combinations are underway, and according to Leopold, this trend will likely continue. Notable combinations include chemotherapy + CPI, VEGFi + CPI, BRAFi/MEKi + CPI, and CPI + CPI.
Such combinations can be difficult to evaluate, suggests Keler. Often, their ability to increase the number of responders is assessed in empirical studies, which can be difficult to interpret. Randomized trials would be clearer.
Biomarker development and precision therapy
“Every cancer patient is unique,” insists Kreiter. “Therefore, each patient’s treatment should be individualized.” Ongoing research is shedding light on several biomarkers that may be good predictors of response to therapies, he adds, but unfortunately, these investigations take time and are quite expensive.
Biomarkers beyond PD-L1 expression are needed to accurately tailor treatments for patients. Eventually, precision treatments may be identified for patients using a distinctly biomarker-driven approach to improve outcomes, Leopold notes. For example, pembrolizumab is approved for the treatment of patients with microsatellite instability-high (MSI-H) or deficient mismatch repair (dMMR) solid tumors that have progressed following prior treatment, regardless of the tumor type.
Cell-based cancer immunotherapies
One of the oldest cell-based cancer immunotherapies is sipuleucle-T, an immunostimulant that is sometimes referred to as a therapeutic vaccine. It was approved by the FDA in 2010 for use against prostate cancer. Despite this success, it is a commercially challenging product, says Kreiter. It requires a complex manufacturing procedure involving the culturing of the patient’s cells, limiting clinical benefits and all but ensuring high treatment costs.
More recently, another kind of cell-based cancer immunotherapy, or adoptive cell transfer (ACT) therapy, has been approved, and it may be more clinically and commercially viable—especially if it assumes autologous form. It’s called chimeric antigen receptor (CAR) T-cell therapy. The CARs in CAR T-cell therapy are genetically engineered receptor proteins that bind to target proteins on cancer cells.
In 2017, the FDA approved a CAR T-cell therapy called axicabtagene ciloleucel for the treatment of diffuse large B-cell lymphoma. In 2018, the FDA approved tisagenlecleucel for adults with certain types of non-Hodgkin lymphoma. Although CAR T-cell therapies are effective against hematological malignancies, they have had less success against solid cancers. The tumor microenvironment is more hostile, fewer specific targets exist, and advances in site-specific delivery and maintenance of therapy are needed.
Ongoing Challenges
If theories and treatment are to be evaluated in human patients, stringent accountability standards are required, Keler emphasizes. Some rules are in place. Nonetheless, more timely and transparent sharing of information from all clinical trials, whether they succeed or not, would benefit the global community. Such sharing needs to be encouraged, given that information may not flow freely in competitive markets.
Leopold also suggests that clinical trials could incorporate endpoints that would help scientists expedite the identification of clinical benefits. Such endpoints could improve decision making in the development of novel therapies, and they could help channel research and resources to promising treatments. In addition, defining approaches to turn uninflamed or “cold” tumors into inflamed or “hot” tumors could lead to better patient outcomes.
Overcoming resistance to treatment remains an ongoing challenge. Serial biopsies of patients and large biobank data utilization could facilitate the identification and targeting of resistance mechanisms.
Future possibilities
The gut microflora controls many body activities. Consequently, the gut microflora’s composition is believed to influence the immune system’s response to immunotherapy. Harnessing the microbiome, then, is an intriguing approach in immunotherapy research.
“Another interesting and rapidly growing area of study is bi- or multispecific agents that combine the targeting of two or more immune pathways into a single drug, for example, two different CPIs or a CPI with a T-cell-activating agent,” says Keler. In addition to posing practical advantages from a development perspective, these molecules can be more potent than combinations of multiple molecules.
Martin concurs that, ultimately, in combination with CPIs and other targeted therapies, bi- or multispecific agents will progress toward human patients. Expect data from this novel class of agents to emerge in the coming years.
Kreiter sees a significant opportunity in using mRNA to carry plans to cells about the expression of therapeutic proteins. If mRNA carriers are suitably engineered, they could target specific tissues throughout the human body.
Although progress may be incremental as the field gathers more data, it is also possible that serendipity may play a role, setting up breakthroughs. It is certainly an exciting time to be involved in cancer research and to have the potential to positively impact a vast number of lives.