Cancer cells don’t follow the rules—at least not the rules of healthy development, growth, and death. Call them lone wolves, rebellious children, or outright criminals, cancer cells behave in uncontrolled ways, often threatening the lives of their biological hosts. Indeed, cancer cells are so resistant to ordinary checks and balances that they often defy understanding.
To make sense of the apparent senselessness of cancer, researchers are using new tools that can more precisely determine how cancer arises, proliferates, and responds to treatment. Single-cell analysis can now identify rare populations of cells and determine their genetic, transcriptomic, and epigenomic behaviors. At the same time, spatial analysis can untangle the cellular architecture of the tumor microenvironment and delineate complex interactions between cancer, immune, and stromal cell populations. These advances do more than deepen our understanding of how cancer cells behave—they open the door to more accurate diagnoses and prognoses, and to more precise, possibly individualized, treatments.
Today, two anticancer approaches are most prevalent in medicine:
- Developing agents that attack tumors and leave healthy tissue alone.
- Arming a patient’s own immune system to do the job of fighting and killing cancer.
Both of these approaches depend heavily on single-cell and spatial analyses.
For the first approach (agents that attack tumors), researchers have used single-cell technologies to make great strides in classifying and categorizing cancers, and in extracting tumor-specific biomarkers that can help drug developers predict which patients are most likely to respond to treatment. Thanks to single-cell analyses, significant findings for nearly every cancer type now allow us to describe cancer-specific gene expression signatures associated with heterogeneous disease phenotypes.
For attack agents, sometimes friends are foes
Patients with B-cell leukemias and lymphomas have benefited from chimeric antigen receptor (CAR) T cells or bispecific T-cell engager (BiTE) antibodies that target CD19, a surface antigen involved with B-cell development and proliferation.1 CD19 is a popular target for CAR T cells and other therapies because it is expressed in various B-cell cancers. Patients with new and relapsed blood cancers have seen highly effective results from CD19-targeted CAR T-cell treatments. In one Phase II study of patients with refractory B-cell lymphoma, 40% of those given CD19-targeted CAR T-cell therapy showed complete remission 15 months later. Other studies showed remission rates of 43% and 71% in patients with large B-cell lymphoma and follicular lymphoma, respectively.
However, this success comes with a catch. Both of the aforementioned studies also reported high incidences of neurotoxicity (64% in the first, 39% in the second). Neurotoxicity reactions included swelling, multifocal hemorrhage, and vascular disruption in the brain. Some of these reactions have been fatal.
To find the reason for neurotoxic reactions, researchers at Stanford University and their colleagues used single-cell RNA sequencing (scRNA-seq) data from human brain cells from the Human Cell Atlas. This large-scale, tissue-wide database of scRNA-seq data helped identify cell populations that were affected by CD19-targeted CAR T-cell therapies.
In a 2020 paper in Cell, the researchers found that CD19 was present in mural cells in the brain.2 Mural cells, including pericytes and vascular smooth muscle cells, surround endothelial cells and regulate the structural integrity of the blood-brain barrier. CD19 mural cell expression was seen in several datasets, in several brain regions, and over many developmental time points. Most important, the CD19 isoforms discovered had the FMC63 epitope targeted by clinical CAR T-cell and BiTE therapies.
Only scRNA-seq could have uncovered the rare populations of brain cells with CD19 expression. “These rare cell types might otherwise be missed in measurements of bulk tissue due to their low frequency, but as we now demonstrate, could be critically important in the clinical effects of targeted therapy,” the researchers wrote.
A need for more markers
The study underlines the need for more sophisticated combinatorial targets and biomarkers for cancer therapies. Indeed, new biomarker discoveries are already being made. In non-small cell lung cancer, the most deadly form of lung cancer, only 20–40% of cancer patients respond to immunotherapy. In addition, dangerous side effects caused by adverse immune system responses restrict the number of patients who can receive cancer immunotherapy in the first place.
Cancer immunotherapy decisions can now be made by assessing expression of PD-L1 on cancer cell surfaces, as well as the tumor mutational burden, which serves as a readout of cancer cell mutations. But recent studies have pointed to the need for biomarkers that resolve the dynamic interplay between the tumor and the immune microenvironment.
A team of scientists at the Icahn School of Medicine at Mount Sinai, New York, used single-cell gene expression, cell surface protein, and T-cell receptor profiling to perform a comprehensive analysis of cancer samples.3 Analyzing 361,929 single cells from 35 tumors, they created the largest single-cell map of early-stage lung cancer immune responses to date.
The researchers found 49 immune clusters among six cell populations (T cells, B cells, plasma cells, mast cells, plasmacytoid dendritic cells, and mononuclear phagocytes). Out of the diverse mix of cells, one cluster was enriched with IFNG, GZMB, LAG3, CXDFL13, and HARCR2 transcripts and increased expression of PD-1, ICOS, and CD39, some of which were directly connected to the underlying mechanisms of immune checkpoint inhibition therapies. Taken together, these data implicate immune cell composition as a potential nonredundant biomarker that could indicate patient response to immunotherapy.
Arming the immune system
Single-cell-based analysis and research can also aid in developing new therapeutics to elicit the body’s immune system to target and kill cancer cells. In 2010, two patients with advanced chronic lymphocytic leukemia (CLL) were infused with their own CAR T cells as part of a University of Pennsylvania Phase I trial.4 Ten years later, as the researchers published in Nature, the patients remained in sustained remission from CLL.5 Remarkably, the patient’s CAR T cells were still detectable a decade after their infusion, while CD19 B cells and CLL cells were not.
How did this happen? The researchers used scRNA-seq and other techniques to find, for the first time, how CAR T cells reacted with other immune system components to produce long-term remission. They found that in the years after infusion, the patients developed a highly activated CD4+ population, which ultimately dominated the population of CAR T cells later on. Single-cell multiomics using cell surface protein and T-cell receptor profiling showed that the CD4+ CAR T cells continued to be cytotoxic, and that they also continued to proliferate, leading to the remission.
Seeing the whole tumor picture
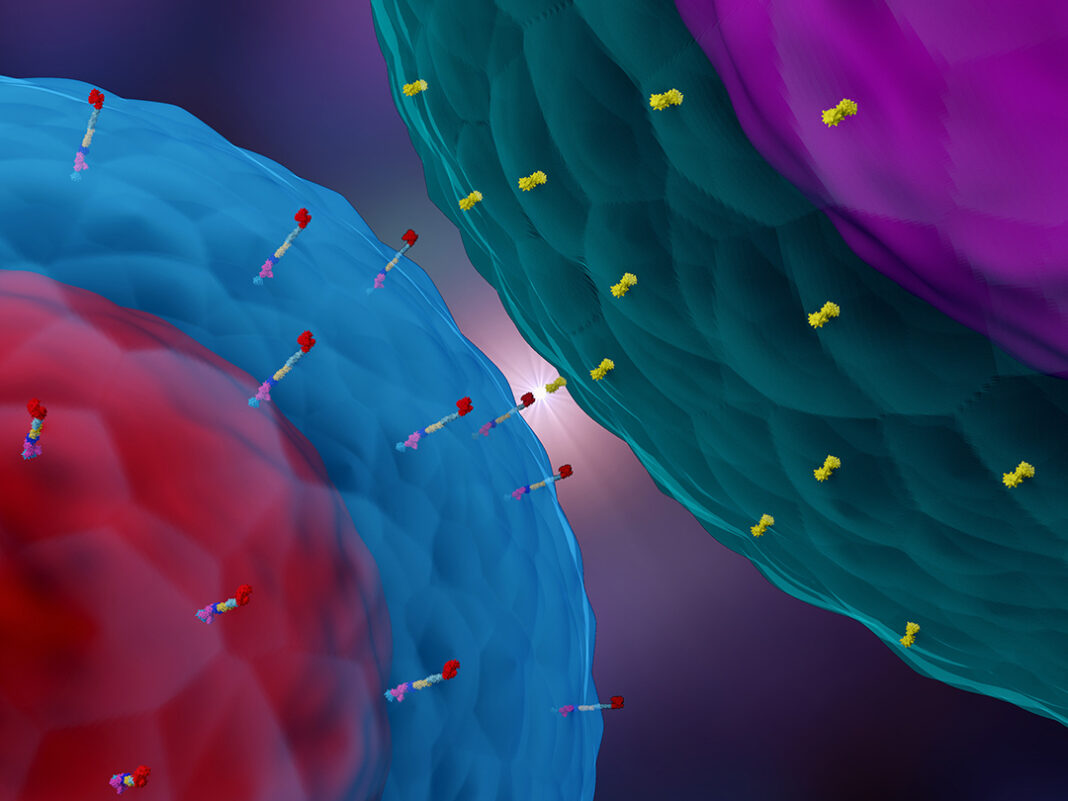
The lesson behind this research is that determining the most effective immunotherapies relies on seeing the tumor microenvironment for what it is: a highly complex, dynamic system of cancer, normal, immune, and stromal populations, all engaging in a cellular struggle on many fronts. Effective therapies should be able to manage this environment to help the immune cell “good guys” quell the cancer cell “bad guys.” Early successes in checkpoint inhibitor and cell therapies demonstrate the incredible potential to be found in harnessing the immune system to fight cancer, but more work is needed to broaden the utility of immunotherapies to more patients and combat resistance.
To finally curb the lawlessness of cancer, we need to fully resolve the complexity of the tumor microenvironment. Single-cell and spatial multiomic tools are critical to develop maps of cellular phenotypes and interactions driving response and resistance to therapies. These insights will enable the development of more combination therapies that take advantage of multiple biomarkers to direct treatments.
References
1. CD19—The Most Popular Target with CAR T-Cell Therapy. Cusabio Technology. Accessed June 2, 2022.
2. Parker KR, Migliorini D, Perkey E, et al. Single-cell analyses identify brain mural cells expressing CD19 as potential off-tumor targets for CAR-T immunotherapies. Cell 2020; 183(1): 126–142.e17. DOI: 10.1016/j.cell.2020.08.022.
3. Leader AM, Grout JA, Maier BB, et al. Single-cell analysis of human non-small cell lung cancer lesions refines tumor classification and patient stratification. Cancer Cell 2021; 39(12): 1594–1609.e12. DOI: 10.1016/j.ccell.2021.10.009.
4. Habern O. Time plus technology reveal secrets of long-lasting CAR T therapy. 10x Genomics. Posted April 12, 2022. Accessed June 2, 2022.
5. Melenhorst JJ, Chen GM, Wang M, et al. Decade-long leukaemia remissions with persistence of CD4+ CAR T cells. Nature 2022; 602(7897): 503–509. doi: 10.1038/s41586-021-04390-6.
Abbey Cutchin is associate director, market development, oncology at 10x Genomics.