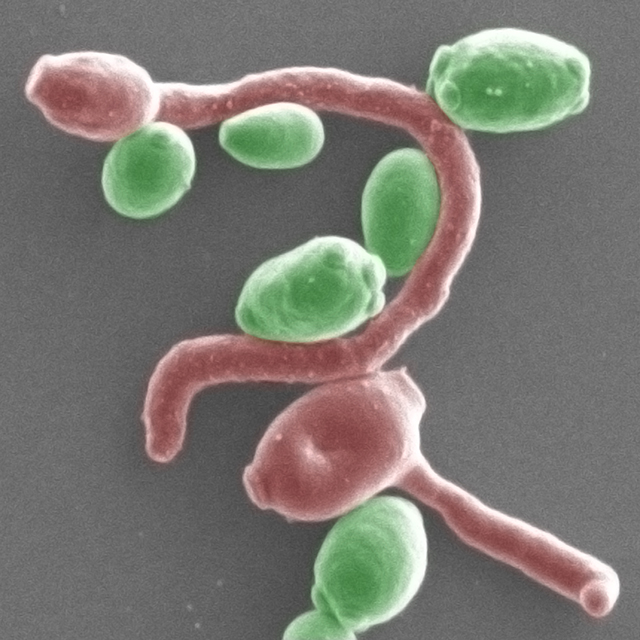
Invasive candidiasis is a life-threatening fungal infection often found in hospitalized patients being treated with antibiotics. The mechanisms underlying this common clinical observation have been unclear until now.
A new study led by Michail Lionakis, MD, ScD, chief of the fungal pathogenesis section at the National Institutes of Health, has found previous exposure to broad-spectrum antibiotics increases susceptibility to Candida albicans infections in mice and affects ensuing immune responses. The researchers found antifungal immunity in the gut was specifically depleted in antibiotic-administered mice, which was compounded by complications arising from bacterial escape and systemic bacterial co-infections.

First author of the study, Rebecca Drummond, PhD, a fungal immunologist at the University of Birmingham, U.K., said, “We knew that antibiotics make fungal infections worse, but the discovery that bacterial co-infections can also develop through these interactions in the gut was surprising. These factors can add up to a complicated clinical situation. By understanding these underlying causes, doctors will be better able to treat these patients effectively.”
The study was published in the journal Cell Host and Microbe, in an article titled, “Long-term Antibiotics Promote Mortality After Systemic Fungal Infection by Driving Lymphocyte Dysfunction and Systemic Escape of Commensal Bacteria.”
Tobias Hohl, MD, PhD, chief of infectious diseases service at Memorial Sloan Kettering Cancer Center, who was not involved in the current study, said, “This work is important because it highlights how an antibiotic can cause damage to the intestinal immune system and render a patient more susceptible to developing a second infection, emphasizing the need for appropriate and judicious use of antibiotics in clinical settings.”
The authors showed that vancomycin decreased a subset of pro-inflammatory T helper cells defined by their production of interleukin 17 (Th17 cells) in mouse models of dysbiosis, where the healthy equilibrium of gut microflora is disrupted.
“We used animal models to analyze how broad-spectrum antibiotics affect systemic immune responses to Candida albicans and demonstrate that pre-exposure to antibiotics, especially vancomycin, disrupt antifungal immunity in an organ-specific manner and that these effects can be ameliorated by targeted immunotherapy,” the authors noted.
“The antibiotic that exerted the greatest effect in mice was oral vancomycin, which is used in humans to treat Clostidioides difficult colitis (C. diff) and is not used to treat systemic bacterial infections since oral vancomycin is not absorbed,” said Hohl. “Thus, the authors convincingly demonstrate that oral vancomycin administration causes an inadvertent injury to the intestinal immune system (likely by destroying beneficial bacteria in the gut) that weakens the immune system’s ability to control fungal disease at this site.”
The authors also analyzed health records of patients between 2009 and 2017 from Cerner HealthFacts, a large de-identified electronic health record database from U.S. academic and community hospitals, to retrospectively analyze relationships between pre-exposure to broad-spectrum antibiotics and invasive candidiasis infections. They found, as expected from their animal studies, pre-exposure to broad-spectrum antibiotics increased risk of invasive candidiasis and decreased survival post-infection.
Immune-boosting drugs prescribed with antibiotics could reduce the health risks from complex infections, the researchers concluded. The team also said the work highlights how antibiotics can have additional effects on our immune system.
“If we limit or change how we prescribe antibiotics we can help reduce the number of people who become very ill from these additional infections—as well as tackling the huge and growing problem of antibiotic resistance,” said Drummond.
In their mouse studies, the authors showed a cocktail of broad-spectrum antibiotics including ampicillin, metronidazole, neomycin, and vancomycin, impaired lymphocyte-dependent IL-17A- and GM-CSF-mediated antifungal immunity in the gut and vancomycin alone could similarly increase susceptibility to invasive fungal infection and systemic bacterial co-infection. IL-17A or GM-CSF immunotherapy prevented systemic bacterial co-infection in these mice, the authors demonstrated in rescue experiments.
“A limitation of the study relates to differences between the mouse model and human study. When the authors administered antibiotics systemically in mice, a common strategy to treat severe infections in humans, they did not observe damage to lymphocyte-dependent intestinal defenses against Candida,” said Hohl. “This result will need further clarification and future work will need to address the role of other commonly used classes of antibiotics in humans, for example, carbapenems, that are administered systemically and have broad activity against gut commensal bacteria.”
Hohl added, “The authors defined specific types of gut commensal bacteria in mice (segmented filamentous bacteria) that induce protective responses in lymphocytes. Because mouse and humans harbor different commensal bacterial communities, the bacteria that may exert similar functions in humans remain undefined.”
Despite these limitations, the findings reported in this study add to growing evidence that antibiotics can disrupt immune function, open avenues for translational immune interventions, and caution against indiscriminate antibiotic use to protect patients from fatal infections and prevent the looming specter of antimicrobial resistance.