![These lung spheroid cells showed powerful regenerative properties when applied to a mouse model of lung fibrosis. [NCSU and UNCSM]](https://genengnews.com/wp-content/uploads/2018/08/147005_web2331173712-1.jpg)
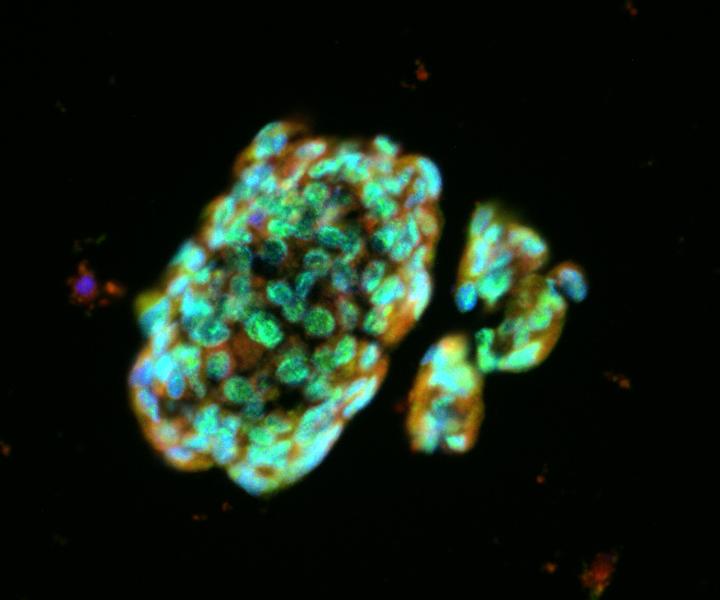
These lung spheroid cells showed powerful regenerative properties when applied to a mouse model of lung fibrosis. [NCSU and UNCSM]
A team of investigators from the University of North Carolina School of Medicine (UNCSM) and North Carolina State University (NCSU) have just released details from a promising study that could potentially offer new stem cell treatment options to patients afflicted with lung conditions such as idiopathic pulmonary fibrosis (IPF), chronic obstructive pulmonary disease (COPD), and cystic fibrosis (CF). Due to the success of this new research, the investigators have been in discussions with the FDA and are preparing an application for an initial clinical trial in patients with IPF.
“This is the first time anyone has generated potentially therapeutic lung stem cells from minimally invasive biopsy specimens,” noted co-senior senior study investigator Jason Lobo, M.D., an assistant professor of medicine at UNC and medical director of lung transplant and interstitial lung disease.
In this new study—published recently in the journal Respiratory Research, in an article entitled “Derivation of Therapeutic Lung Spheroid Cells from Minimally Invasive Transbronchial Pulmonary Biopsies”—the researchers were able to demonstrate that they could harvest lung stem cells from people using a relatively noninvasive doctor's office technique. Consequently, the scientists were then able to multiply the harvested lung cells in the lab to yield enough cells sufficient for human therapy.
This new evidence was based upon previous work done by these investigators, published in Stem Cells Translational Medicine, where the authors provided clear evidence that using a rodent model of IPF—a chronic, irreversible, and ultimately fatal disease characterized by a progressive decline in lung function—could be successfully treated with the same type of lung stem cell as generated in the current work.
“We think the properties of these cells make them potentially therapeutic for a wide range of lung fibrosis diseases,” explained co-senior study investigator Ke Cheng, Ph.D., an associate professor in NCSU's department of molecular biomedical sciences and the UNC/NCSU joint department of biomedical engineering.
Currently, the two FDA-approved drug treatments for IPF reduce symptoms but do not stop the underlying disease process. The only effective treatment is a lung transplant, which carries a high mortality risk and involves the long-term use of immunosuppressive drugs. These diseases of the lung involve the buildup of fibrous, scar-like tissue, typically due to chronic lung inflammation. As this fibrous tissue replaces working lung tissue, the lungs become less able to transfer oxygen to the blood. Patients ultimately are at risk of early death from respiratory failure. In the case of IPF, which has been linked to smoking, most patients live for fewer than five years after diagnosis.
In the current study, the research team set their focus on a set of stem cells and support cells that reside in the lungs and can be reliably cultured from biopsied lung tissue. The cells are called lung spheroid cells for the distinctive sphere-like structures they form in culture. Previous studies showed that lung spheroid cells have powerful regenerative properties when applied to a mouse model of lung fibrosis. In their therapeutic activity, these cells also outperformed other non-lung-derived stem cells known as mesenchymal stem cells, which are also under investigation to treat fibrosis.
The scientists showed that they could obtain lung spheroid cells from human lung disease patients with a relatively noninvasive procedure called a transbronchial biopsy. “We snip tiny, seed-sized samples of airway tissue using a bronchoscope,” Dr. Lobo remarked. “This method involves far less risk to the patient than does a standard, chest-penetrating surgical biopsy of lung tissue.”
Once isolated, the researchers cultured lung spheroid cells from these tiny tissue samples until they were numerous enough—in the tens of millions—to be delivered therapeutically. When they infused the cells intravenously into mice, they found that most of the cells gathered in the animals' lungs.
“These cells are from the lung, and so in a sense, they're happiest, so to speak, living and working in the lung,” Dr. Cheng stated. “The treatment was safe and effective whether the lung spheroid cells were derived from the recipients' own lungs or the lungs of an unrelated strain of rats,” Lobo said. “In other words, even if the donated stem cells were foreign, they did not provoke a harmful immune reaction in the recipient animals, as transplanted tissue normally does.”
The researcher’s expectation is that when used therapeutically in humans, lung spheroid cells initially would be derived from the patient to minimize any immune-rejection risk. Ultimately, however, to obtain enough cells for widespread clinical use, doctors might harvest them from healthy volunteers, as well as from whole lungs obtained from organ donation networks. The stem cells could later be used in patients as is or matched immunologically to recipients in much the same way transplanted organs are typically matched.