Scientists in the U.S. have demonstrated how modified strains of Zika virus can prolong the lifespan of mice with glioma by specifically targeting and killing cancer stem cells that drive tumor progression. Studies by researchers at Washington University School of Medicine (WUSM) in St. Louis, the University of California, San Diego (UCSD), and the Cleveland Clinic Lerner Research Institute, showed that Zika virus preferentially targets and kills proliferating glioblastoma stem cells (GSCs) in human glioblastoma cell lines, in human brain tumor tissue, and in tumor-bearing mice without affecting healthy neural cells or differentiated glioblastoma cells (DGCs). “Zika very specifically killed brain tumor stem cells with little effect on differentiated tumor cells and adult neural cells,” explained Jeremy Rich, M.S., one of the team leaders at UCSD and the Cleveland Clinic Lerner Research Institute, speaking with GEN.
The researchers suggest that their studies represent a starting point for the development of safe oncolytic Zika virus strains that could be exploited as part of a two-pronged anticancer treatment approach that combines cytotoxic drugs to kill differentiated tumor cells, with Zika virus therapy to target and destroy the proliferating, treatment-resistant GSCs.
Dr. Rich and WUSM colleagues Milan Chheda, M.D., and Michael Diamond, M.D., Ph.D., who co-led the research, published their findings today in the Journal of Experimental Medicine, in a paper entitled, “Zika Virus Has Oncolytic Activity against Glioblastoma Stem Cells.”
Glioblastoma is the most common form of brain cancer, and most patients will die within two years of diagnosis, at least in part because proliferating GSCs survive traditional cancer therapy and immune system attack and drive disease progression, even after chemotherapy has destroyed the bulk of differentiated tumor cells. There are numerous similarities between these GSC cells and the neural stem and progenitor cells in the developing fetal central nervous system that the Zika virus infects and destroys, Dr. Rich commented to GEN. “GSCs are functionally defined based on many stem/progenitor behaviors—self-renewal, stem cell marker expression, sustained proliferation, ability to recapitulate the tissue from which they were derived. The chromatin state of both can be very similar. A major difference is that neural precursors respond to their environment and stop growing when told to do so.”
It was this similarity between fetal neuroprogenitors, and GSCs that led Zhe Zhu, Ph.D., a postdoctoral fellow in Dr. Rich’s group and lead author of the JEM paper, to consider the potential use of Zika virus to target and destroy tumor-specific stem cells in glioblastoma. “Zhe hypothesized that findings from studies investigating how Zika virus attacks fetal neuroprogenitors could signal that brain tumor stem cells, which activate many pathways similar to early stage neuroprogenitors, could also be affected by Zika infection,” Dr. Rich added. “We sought out collaborators with complementary expertise, and this led to a remarkable multi-group partnership.”
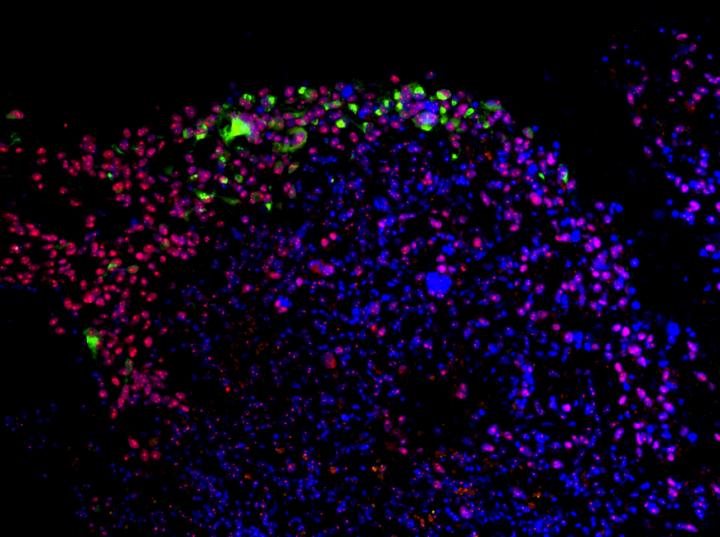
The team first demonstrated that different strains of Zika virus specifically targeted and killed GSCs in cultures of patient-derived glioblastoma cells, but also in samples of freshly excised human glioblastoma tissues. In contrast, the virus didn’t infect differentiated human neural stem cells, or DGCs, in patient-derived cultures or in normal adult human brain tissue specimens to any great degree. This specificity for GSCs appeared to be unique to Zika virus. The related flavivirus, West Nile virus, was found to be less selective and infected and killed both cultured GSCs and DGCs. Interestingly, about 65 years ago, West Nile virus had been tested as a potential oncolytic virus, but demonstrated “substantial toxicity,” the authors at that time wrote. “The exciting and surprising finding was that Zika was very different than West Nile Virus, which is from the same family, but had broad targeting, which likely explains the toxicity of the original West Nile cancer trials,” Dr. Rich suggested to GEN. “Thus, Zika could be a better platform to build on for developing oncolytic viruses with acceptable toxicity.”
Mice are not natural hosts for Zika virus, so to progress their studies into an in vivo model, the researchers had to develop a mouse-adapted strain of Zika virus. They first used this modified virus to infect mouse glioma cells and normal mouse central nervous system cell lines in vitro. As expected, the mouse-adapted Zika virus infected and held back glioma cell growth, without affecting differentiated central nervous system cells.
The researchers next tested the mouse-adapted Zika virus in animals bearing mouse gliomas. Just a week after treatment, tumors in the control animals had grown much larger than those in the Zika virus-treated mice. Tumors in the infected animals demonstrated significant levels of cell death, and the Zika virus-treated mice also lived longer than the control animals.
Encouragingly, a recombinantly derived attenuated Zika virus strain (ZIKV-NS5 E218A) was just as effective against three human GSC in vitro models as a wild-type Zika virus, but demonstrated limited replication capacity. Treating these cultured cells with a combination of ZIKV-NS5 E218A and standard-of-care chemotherapy temozolomide—to which GSCs are commonly resistant—resulted in much greater antitumor effects than temozolomide alone. This suggests that that combination therapy might prove an effective approach against glioblastoma, the authors note. They also suggest that the E218A mutant virus might represent “a framework for further genetic modification to ensure safety and maintain efficacy.”
The researchers acknowledge that we don’t yet know how Zika virus strains will act on patient-derived GSCs in vivo. “This will require overcoming the technical challenges of creating patient-derived tumor models in more immunocompetent mice.” Nevertheless, they write, “our work serves as a foundation for further mechanistic studies and the genetic engineering of a safe and effective ZIKV, which could become an important tool in neuro-oncology.”
The group is also now working to evaluate the potential use of Zika virus against other types of cancer and is also developing a drug screen “to augment efficacy as a combined treatment paradigm,” Dr. Rich stated. Oncolytic viruses have previously been used to treat patients, and there have been some promising results, “but we hope to add to the arms race against this cancer…as a neuro-oncologist, I want to put myself out of business,” he told GEN.
Combining the team’s findings with those of previous research has thus provided new insights into Zika virus infection, Dr. Rich stressed. “West Nile Virus affects both adults and younger individuals, whereas Zika is more (but not exclusively) pathogenic against patients at an earlier development stage. These findings have provided clues that we are following to understand why this process is selective, which may direct the development of an improved modified virus.”
And although scientists still don’t understand the mechanism by which Zika virus preferentially targets GSCs, the team’s RNA sequencing studies on GSCs and DGCs identified a group of differentially expressed immune genes, including type I interferon (IFN)-stimulated genes (ISGs) that were upregulated in DGCs. They found that Zika virus-infected GSC models also triggered IFN signaling. And when DGCs were treated with an antibody that blocked IFN-alpha/beta receptor 2 (IFNAR2), the cells became more susceptible to Zika virus infection. “So far, our results suggest that GSCs have differences in their immune responses,” Dr. Rich indicated to GEN. “This can cause both cell autonomous and systemic effects. This tells us that we can modify the virus based on the mutant form that we described to create even greater selectivity. It also may suggest that combinations with oncoimmune therapies may have additional benefit.”