![Scanning electron microscope image of breast cancer cell. New evidence suggests a weak immune response is associated with recurrence of these tumors. [National Cancer Institute, NIH]](https://genengnews.com/wp-content/uploads/2018/08/Jan4_2016_NIH_BreastCancerCell6137186194-1.jpg)
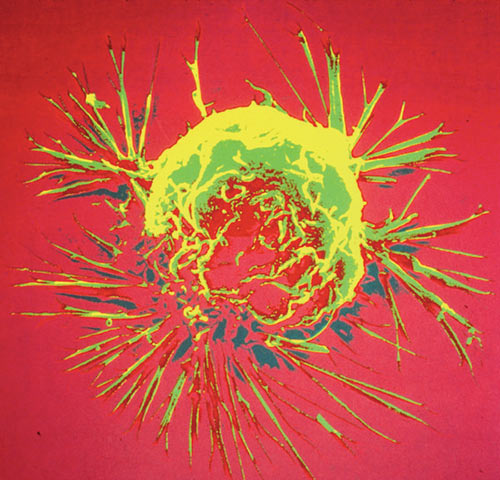
Scanning electron microscope image of breast cancer cell. New evidence suggests a weak immune response is associated with recurrence of these tumors. [National Cancer Institute, NIH]
In the past several years researcher have made a number of significant advances in cancer treatments through advanced detection methods and new drug therapies. However, due to the complex heterogeneity that comprises most tumors, complete eradication of all cancer cells, especially for breast cancer, is still proving to be tough.
Now, scientists from the University of Pennsylvania Perelman School of Medicine believe they have found evidence that recurrence of HER2-positive breast cancer after treatment may be due to a specific and possibly cancer-induced weakness in the patient's immune system. The researchers are hopeful that this evidence could lead to new targeted chemotherapies or a possible HER2-targeted vaccine.
The results of the current study also suggest that patients with HER2-positive breast cancer may, in the near future, undergo immune status monitoring using blood tests before, during, and after treatment to allow physicians to gauge the risk of recurrence, and possibly to reduce that risk with therapies that boost anti-HER2 immunity.
“We know that it's not a fixed immune defect, because we have several clinical trials open where we're vaccinating people and can restore anti-HER2 responsivity,” explained senior study author Brian Czerniecki, M.D., Ph.D., professor of surgical oncology at Penn and the co-director of the Rena Rowan Breast Center at Penn's Abramson Cancer Center.
Dr. Czerniecki and his colleagues isolated immune cells from 95 women with invasive HER2-positive breast cancer and analyzed the ability to mount a pro-inflammatory (Th1) response against the HER2 growth factor receptor protein, which drives the tumor’s rapid proliferation.
The findings from this study were published recently in JAMA Oncology through an article entitled “Association of Depressed Anti-HER2 T-Helper Type 1 Response With Recurrence in Patients With Completely Treated HER2-Positive Breast Cancer.”
Additionally, the researchers found that cells from women with recently recurrent cancer that had not yet been re-treated had only about a tenth of the anti-HER2 responsivity as compared to women whose HER2+ breast cancer had not recurred for at least two years following treatment.
Subsequently, when the team looked at anti-HER2 responsivity across all patients they found that those with the least amount of responsivity had experienced only 47 disease-free months after treatment, on average, compared to 113 disease-free months for the patients with the most responsivity. Moreover, they found that low anti-HER2 T cell response in recurrent patients was not part of a broader immune suppression.
“We detected no other immune deficit—just the deficit in the anti-HER2 response,” Dr. Czerniecki noted.
The results from this study complement previous findings from this group, which found that immune system response against HER2 varied widely in cancer-free patients versus early-stage HER2-positive patients. The mechanism for how individuals lose their anti-HER2 responsivity remains elusive, but is an area that the Penn scientists are actively pursuing.
“The thinking is that the patient's anti-HER2 T cells somehow become exhausted and die or otherwise stop responding,” Dr. Czerniecki stated. “We're trying to determine the mechanism, but we already know that we can 'fill the tank' with vaccines to restore that specific responsivity to HER2.”