Heather Lau, MD, is an expert in mucopolysaccharidoses (MPS), having dedicated much of her career as a pediatric neurologist to treating patients with these rare inherited lysosomal storage diseases.
As the director of New York University’s (NYU) Langone Health’s Division of Neurogenetics and Lysosomal Storage Disorders Program, Lau was in charge of the clinical trials for this large, rare disease population.
“I was running trials of protein, small molecule, and gene therapy at NYU for many years,” Lau told GEN Edge. “That was a passion, especially getting my patients through COVID-19.”
However, Lau started to get frustrated with the lack of drug development progress in the neuropathic MPS space.
“We have some effective therapies for the non-neuropathic lysosomal storage diseases, such as Gaucher, Fabry, and Pompe, and we have enzyme replacement therapy for MPS IVA and VI, which do not have neurologic problems—they have a severe system burden,” said Lau. “But in a disorder like MPS IIIA, also known as Sanfilippo syndrome type A, the main clinical manifestations are neurologic and cognitive.”
Lau then joined her MPS mentor and colleague Emil D. Kakkis, MD, PhD, who is known for being very patient-oriented at a company he had founded called Ultragenyx, a biopharmaceutical company focused on drug development for rare and ultra-rare diseases.
As executive director of global clinical development at Ultragenyx, one of Lau’s roles is leading the Transpher A study assessing the AAV-based gene therapy UX111 for treating patients with Sanfilippo syndrome type A (MPS IIIA).
Lau shared the most recent results from Ultragenyx’s Transpher A study, which started as a Phase I/II study but later turned into a Phase III open-label dose escalation study. These results show that the drug is biochemically and functionally effective at improving cognitive function in 17 children with MPS IIIA, a fatal neurodegenerative disorder in children that affects language, motor skills, and thinking.
MPS IIIA flies under the radar
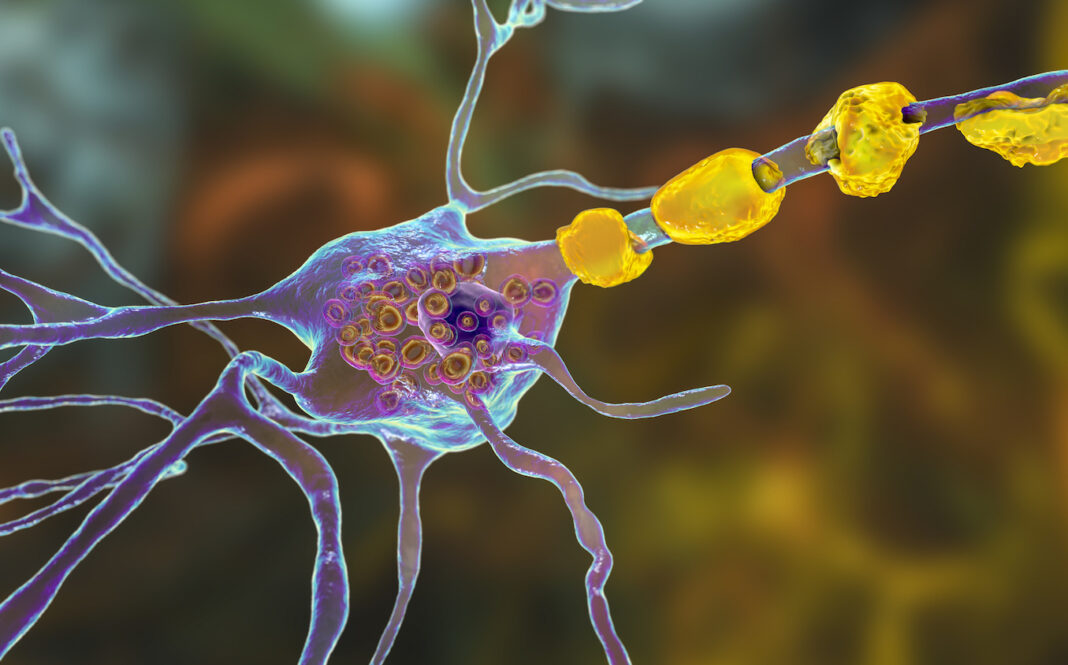
All MPS diseases are characterized by single enzyme defects that lead to the accumulation of long polysaccharides known as glycosylglycans (GAGs), of which there are several types. In MPS IIIA, the GAG that accumulates is heparan sulfate due to mutations in N-sulfoglucosamine sulfohydrolase (SGSH).
According to Lau, the levels of heparan sulfate should be essentially nonexistent in cerebrospinal fluid (CSF), but they do go up and down. But an accumulation of heparan sulfate becomes toxic, causing autophagic derangement, mitochondrial dysfunction, and inflammatory responses in neurons, and a sustained accumulation causes progressive neuronal death.
“You have to look at it—not just the final point, but look at it over time,” said Lau. “Heparan sulfate reduction, if you can imagine, is like a reduction in a toxin, like lead poisoning or phenylketonuria (PKU)—it is all about how long you’re exposed to a toxin. It is not like carbon monoxide poisoning, which is acutely toxic. We’re talking about chronic exposure over time.”
In MPS IIIA, the heparan sulfate builds up from birth through the first couple of years of life, but there’s no real indication until it becomes too late. According to Lau, children with MPSIIIA may learn normally and have normal development—it could be slightly delayed. Still, their trajectory has a positive upward slope, meaning they’re gaining skills. These children learn to walk and talk for the first two years of life and don’t have the characteristic dysmorphology of MPS.
“We don’t have an indicator that there’s something wrong, but then they start to slow down in their development,” said Lau. “As a parent, you’re not losing skills, but they’re not gaining any. So, [parents] start talking to their pediatrician, but [the pediatrician] may not be able to make the diagnosis. Between two and four, they slow down, and after four, they start to lose skills. That really is a red flag for a clinician to say what is happening here? It’s neurodegenerative at this point. So, what we’re trying to do is at the minimum halt the progression and at best actually help keep them on that upward trajectory of development.”
UX111 and newborn screening needs
UX111 is dosed in a one-time intravenous infusion using a self-complementary AAV9 vector to deliver a functional copy of the SGSH gene to cells of the nervous system and peripheral organs.
At the WORLDSymposium™ 2024 20th annual research meeting in San Diego, Ultragenyx is presenting data demonstrating that UX111 is safe, with a top dose of viral genomes (3×1013 vg/kg), which is below dose-limiting toxicities. The most frequently reported treatment-related adverse events to date were elevations in liver enzymes, and the majority of these events were mild (Grade 1) or moderate (Grade 2) in severity. As of now, the only side effect related to the treatment that was Grade 3 (severe or medically significant but not immediately life-threatening) was an increase in alanine aminotransferase (ALT) that went away. This is a known effect of AAV gene therapy.
In terms of biochemical efficacy, they see a mean reduction in CSF heparan sulfate exposure of 63% in the time-normalized area under the curve (AUC). But what Lau is excited about is that they see a statistically significant relationship between sustained reductions in heparan sulfate levels and sustained cognitive benefit in 15 of their 17 patients.
In addition to developing safe and effective gene therapies, treatment of any MPS, including Sanfilippo syndrome type A, involves the identification of gene defects as early as possible.
According to Lau, pathogenic variants are known, and with their new way of understanding the clinical significance of heparan sulfate levels, they can look at unknown variants for pathogenicity by measuring enzyme and substrate levels.
But the major hurdle isn’t necessarily the science—it’s the regulatory nature of developing drugs and screens.
“This is so easy to identify on a newborn screen, but to get to a newborn screen, you have to have disease-modifying therapy,” said Lau. “It is hard because this entire community knows how to identify this disease, and if we identify it earlier by doing mass screenings at the newborn screening level, we could pick it up and intervene. We don’t want to wait until you start to lose skills. There’s no question about how to diagnose this. Everyone would benefit from an early diagnosis and intervention before the brain is impacted.”
The UX111 program, which Ultragenyx acquired from Abeona Therapeutics in 2022, has received Regenerative Medicine Advanced Therapy, Fast Track, Rare Pediatric Disease, and Orphan Drug designations in the United States and PRIME and Orphan medicinal product designations in the EU.
While Ultragenyx has its work cut out, it could be another win for the gene therapy community.