For close to two decades, Draper has worked to develop organ-on-chip technologies designed to speed up drug R&D by eliminating the need for animal studies or culture models using animal or human cells.
Among the organs Draper has worked to model are the lungs—an effort that positioned the company well when SARS-CoV-2 began to wreak havoc on the world nearly two years ago.
“When the pandemic hit, we were ready with technology that could be applied to COVID-19 because of our prior work in other respiratory viruses,” Jeffrey T. Borenstein, PhD, a biomedical engineer and Laboratory Fellow at Draper, told GEN Edge.
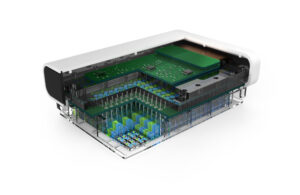
PREDICT96 is a multiplexed single organ system equipped with 96 individual wells and 192 integrated pumps that circulate fluid through a system of fluid channels; sensors monitor individual organs. A blood substitute keeps lung-on-chip tissues alive and is used to circulate compounds and therapies of interest to these artificial organs. Channels guide these agents to tissues, with sensors measuring temperature, pH, oxygen levels and other metrics in real time.
“The platform technology itself is really something that extends or applies to many different organs and disease areas,” Borenstein said. “For the lung it’s set up as an air-liquid interface, so it mimics the way that the airway interfaces with the air passing by and the exposure to respiratory or airborne viruses.”
“The goal is really to accelerate and improve the accuracy and speed and reduce the cost of drug development,” he added.
PREDICT96 is now in “seven or eight” laboratories of biopharma companies that partner with Draper, added David O’Dowd, Draper’s Director, Biomedical Solutions.
Through the Biomedical Advanced Research and Development Authority (BARDA) and its Division of Research, Innovation, and Ventures (DRIVe), the U.S. Department of Health and Human Services (HHS) has awarded Draper a $719,000 federal contract to design a model for human airway tissue and adapt PREDICT96 to collect data for SARS-CoV-2 infection studies.
Draper’s contract (“A High-Throughput and Immune-Competent Lung-on-Chip with Integrated sensing for SARS-CoV-2 Analysis,” PIID 75A50121C00076) calls for developing a custom-engineered 96-device platform called PREDICT96-AIR that can be used to grow and test human primary airway epithelial cells.
The funding comes from the ImmuneChip+ program launched in March by BARDA and the NIH’s NIH’s National Center for Advancing Translational Sciences (NCATS). The goal of ImmuneChip+ is to develop a set of mature “ImmuneChips” that combine a previously validated model of a vital human tissue—such as the lung, the heart, or the kidney—with an immune system component in a single platform that can be machine-manufactured and includes multiple in-line sensors for long-term tissue monitoring.
“Useful Tools”
“With this program, we aim to further enhance the usability of tissue chips and position them as useful tools in the drug development process and for personalized therapeutics,” BARDA and NCATS state on the ImmuneChip+ website.
Draper’s Biomedical Engineering Division in Cambridge, MA, is one of three non-governmental organizations working with BARDA and NCATS to advance tissue chips technology, also called microphysiological systems (MPS), through ImmuneChip+.
The other two organizations are the Vunjak-Novakovic Laboratory at Columbia University; and the Ingber Lab at the Hansjörg Wyss Institute for Biologically Inspired Engineering at Harvard University.
The Vunjak-Novakovic Lab, headed by Gordana Vunjak-Novakovic, PhD, is developing and validating a modular tissue chip system designed to enable studies of human immune responses to respiratory viral infection. The platform will enable modeling of the effects of coronavirus infection on different tissues over many weeks, including immune responses to the virus and the resulting tissue damage. The lab aims to advance the capabilities of tissue chip technology as well as to enable personalized medical studies of patient-specific immune behaviors.
At Wyss, the Ingber Lab headed by Donald E. Ingber, MD, PhD, (the founding director of the Institute) is developing and validating a Human Lymphoid Follicle Chip (LF Chip) with in-line biomarker sensing. The platform is envisioned as potentially aiding in vaccine development by speeding up preclinical evaluation of vaccines and adjuvants. Wyss has previously shown that LF Chips could mimic the effects of vaccination on the human immune system in vitro. Ingber’s “Organ-Chip” technology was named among Top 10 Emerging Technologies of 2016 by the World Economic Forum.
Ingber is scientific founder, board member, and Scientific Advisory Board chairman of Emulate, which was founded to commercialize the Organ-Chip tech. Last month, Emulate completed an $82 million Series E financing, bringing the company’s total capital raised to date to nearly $225 million.
The Charles Stock Draper Laboratory is a nonprofit R&D lab based in Cambridge, MA. Draper finished the 2020 fiscal year ending June 26 with more than $672 million in operating revenue, up 7% from $626 million the previous year. An FY 2021 financial statement had yet to be released at deadline.
Draper’s organ-on-chip efforts began when it worked with drug companies to develop a model of the liver and its complex vasculature: The liver has a dual blood supply consisting of a portal vein that provides two thirds of blood flow to the liver.
The company’s organ-on-chip work expanded into the lungs following interest from government agencies and commercial partners interested in fighting influenza, since annual epidemics have led to the loss of thousands of lives in the U.S. and worldwide—death tolls that multiplied during flu pandemics in 1968 (H3N2 virus) and 2009-10 (H1N1 virus).
“Really Interesting Technology”
Draper was first, Borenstein said, to culture mammalian cells in a microfluidic device about 20 years ago. Over the first 10 years, Draper developed a platform capable of sustaining living human tissue that behaved in key ways like a human. That platform, called Barrier-Immune-Organ: Microphysiology, Microenvironment Engineered TIssue Construct Systems (BIOMIMETICS), was designed to better predict drug efficacy and toxicity in humans during lab testing.
“BIOMIMETICS was really interesting technology,” Borenstein recalled. “But instead of multiplexing an individual organ, we were connecting maybe one or two circuits of interconnected organs, which was a problem that DARPA and NIH were interested in at the time.”
The beauty of PREDICT96, he added, is its ability to scale up the number of replicates and conditions that can be studied for an individual organ model such as the lung.
“But then with BARDA, we’re looking at extending it in at least a couple of directions: One is integration of the immune system, which was really not present in BIOMIMETICS or in any of the systems that were being developed by anybody at that time,” Borenstein said. “The other dimension is to make the systems smarter in the sense that you’re now gathering information: You have on-board, real-time sensing that helps you monitor the data that’s coming out of these systems.”
For the current lung-on-chip effort, Draper cannot carry out COVID-19 research as it has with influenza, since flu studies can be carried out in any number of industry or academic labs, while COVID-19 work limits the company to labs that are Biosafety Level 3 or higher.
Lab Partner
“Draper had to go and arrange for a BSL-3 or an environment that enables higher containment work to be done with the COVID-19 virus,” Borenstein said.
Draper has addressed that need by partnering with the Cummings School of Veterinary Medicine at Tufts University to use its BSL-3 lab.

“People had to be trained, there were all these protocols, so there were a lot of obstacles to putting everything in place,” O’Dowd said. “In addition to the technology, there was a lot of biological work, a lot of preparation work that needed to be done. And luckily we’ve put all those things in place even before this award, not just training.”
O’Dowd, Borenstein, and colleagues will work on characterizing how SARS-CoV-2 and other infections affect the lungs, as well as evaluating the chip’s usefulness in developing therapies for related respiratory pathologies as well.
According to Draper, its lung-on-chip can be used to model healthy and diseased tissue, measuring immune system activity and response to drugs or toxins.
To develop an organ-on-chip, human cells are used to manufacture 3D organ-like structures. These small structures mimic the function of organs such as the liver, kidney, gut and, in this case, the lungs.
Beyond COVID
Early in the COVID-19 pandemic, Draper shut down for two weeks in late March 2020, reopening March 30 of that year for personnel that needed to work in its labs.” we continued projects, we signed new projects, we started new projects, we completed projects. There’s nothing that I can recall that was significantly delayed by COVID. We were kind of fortunate in that regard.”
One result of the pandemic was increased attention among customers for technologies against respiratory diseases, added Timothy Petrie, Principal Member of Technical Staff at Draper: “That includes not only COVID, but all of those diseases, including respiratory distress syndrome. We actually developed new models during the pandemic time for that application.”
Outside of PREDICT96 and the ImmuneChips project, Draper is developing an advanced version of an artificial lung technology called extracorporeal membrane oxygenation (ECMO) designed to more closely mimic human lungs by addressing complications such as blood clots and a resulting need for high levels of anticoagulants.
Borenstein is among staffers working on the engineered biomimetic microfluidic blood oxygenator or “BLOx,” which according to Draper could transform how ECMO is carried out. Draper has won a $4.9 million U.S. Army grant set to run through July 2022 toward developing BLOx.
Another driver of COVID-19 model development has been biopharma’s shift from the race for vaccines to the development of drugs to treat the virus and related diseases—a shift reflected in Merck & Co.’s announcement Friday of positive Phase III data for its oral antiviral candidate molnupiravir.
When I think about our conversations with our pharma partners, we like them kind-of felt, ‘Oh, the vaccines will be developed, the vaccines will get out, the vast majority of people will get it, and then we’re done. It’s becoming more clear, it seems to me, that this might become endemic and just we’re always dealing with COVID,” O’Dowd said.
“Pharma is starting to move towards ‘Alright, there is going to be another market for COVID treatment, so we’re going to have to start thinking about what therapies we can develop, and that’s where our models will come in,” O’Dowd said. “The pull from the market has very much been on models to aid efficacy, not so much safety, but really efficacy—help us figure out if this is going to work or not before we even start animal studies.”
Those models, he said, will need to look beyond vaccines and acute COVID treatment, but long-haul COVID treatments that offers insight into how those syndromes develop and what can be done to prevent and treat them.
Studies Detail PREDICT96
Draper researchers first detailed the PREDICT96 platform in a study published April 21 in the journal Lab on a Chip. Joe Charest, PhD, head of strategy and business development, pharmaceutical R&D technologies at Draper, led a team of researchers from Draper, Pfizer, and Boston University that carried out proof of concept experiments demonstrating the platform’s ability to monitor tissue metrics that included gene and protein expression, oxygen consumption and barrier function.
PREDICT96’s advanced culture capabilities were shown to support a variety of human tissue models including liver, vascular, gastrointestinal, and kidney. “The format is compatible with existing life science tools, including liquid and plate handling tools and assays, such as multiplex immunoassays, HCS and RNA-seq,” Charest and colleagues reported.
Charest and colleagues from Draper, Pfizer, and Raytheon BBN Technologies showed in a study published June 9 in Scientific Reports that PREDICT96 was compatible with several assays, including macromolecular permeability, image-based screening, Luminex, and qPCR.
Two weeks later, in a preprint posted June 23 on bioRxiv, Borenstein and colleagues from Draper and Massachusetts General Hospital reported the first successful demonstration of SARS-CoV-2 infection and viral replication in a human primary cell-based organ-on-chip, using a custom version of PREDICT96 (PREDICT96-ALI) that integrated human primary airway epithelial cells derived from a living donor, in an air-liquid interface.
Borenstein and colleagues from Draper, Massachusetts General Hospital, and University of Massachusetts Medical School further detailed in a study published July 22 in Scientific Reports how PREDICT96-ALI was applied to influenza A virus and another coronavirus infection, HCoV-NL63, in addition to SARS-CoV-2, with researchers evaluating viral infection kinetics and antiviral agent dosing across multiple strains and donor populations of human primary cells. In the custom platform, tissues were cultured in an array of microchannel-based culture chambers at an air–liquid interface.
“This new capability can be used to address a major gap in the rapid assessment of therapeutic efficacy of small molecules and antiviral agents against influenza and other respiratory viruses including coronaviruses,” Borenstein and colleagues wrote.



