April 15, 2016 (Vol. 36, No. 8)
Translational Scientists Profile Cancer Cells That Have Gone on the Lam
For most malignant tumors, morbidity and mortality are, to a great extent, the result of metastatic dissemination, as opposed to the presence of the primary tumor.
The existence of circulating tumor cells, which can be shed into the circulation by primary or metastatic malignancies, was first recognized almost 150 years ago, and their diagnostic and therapeutic values have been increasingly appreciated during the last few decades.
One of the unique characteristics of circulating tumor cells is that they are in a fundamentally different environment from that established in either the primary tumor or the metastatic one. Although circulating tumor cells can be kept in place so that they can be assessed, the usual technique—immobilization to a solid surface—tends to yield distorted results. Free-floating cells are molecularly and functionally distinct from immobilized cells. For example, nonadhering breast cancer cells were shown to have tubulin-based microtentacles that shape their dynamic behavior, including their aggregation, retention in organs, or interaction with the endothelium.
“These microtentacles are very hard to study because they depolymerize when cells bind either an endothelial cell or another tumor cell,” says Christopher M. Jewell, Ph.D., assistant professor of bioengineering at the University of Maryland College Park. “Cells that form microtumors undergo massive mechanochemical and phenotypic changes as compared to when they are floating or circulating.”
Characterizing circulating tumor cells, then, seems to amount to capturing the substance of freedom, a task that sounds self-defeatingly paradoxical—or at least fraught with difficulties. Overcoming difficulties, however, would likely be worth the effort. Two areas that immediately benefit from the characterization of circulating tumor cells are diagnostics and therapeutics.
Capturing and analyzing circulating tumor cells opens not only the possibility of diagnosing patients earlier and more accurately, but also the potential for identifying new approaches to targeting malignancies. “Many groups are working on important technologies to capture circulating tumor cells,” informs Dr. Jewell. “We’re working on new technologies to analyze these populations.”
Floating in Place
To address the existing gap in characterizing the biology of free-floating cancer cells, Dr. Jewell and collaborators in the University of Maryland laboratory of physiologist Stuart Martin, Ph.D., have designed an unusual microfluidic device. It can spatially immobilize free-floating tumor cells while maintaining their free-floating characteristics.
In this microfluidic device, polyelectrolyte multilayers inhibit the attachment of cells to multiwall plates, allowing their free-floating functional and morphological characteristics to be visualized and studied. Lipid tethers incorporated into the device interact with the cell membrane and allow cells to remain loosely attached and spatially localized, offering the possibility to perform applications such as real-time imaging and drug screening.
“We are trying to understand what the signaling changes are in individual circulating tumors cells that are not nucleating into a tumor,” explains Dr. Jewell, “as compared to cells that contact enough cells and nucleate to form a tumor.”
Surface tethering of circulating tumor cells also provides the opportunity to capture arrays of tumor cells; to introduce a perturbation such as a drug or a change in flow rate or mechanical properties; and then to collect the same individual cells that had already been imaged. In these cells, morphological changes can be correlated with genomic or proteomic information, providing an opportunity to dynamically understand how the mechanochemical properties of the cells change in response to external perturbations.
“Our collaborators,” notes Dr. Jewell, “are also developing algorithms to quantify some of the features of microtentacles and convert visual information into quantitative metrics.”
Filterless Filters
Early techniques to capture circulating tumor cells have taken advantage of cell size differences, leading to the development of filtration-based approaches. This was followed, more recently, by the emergence of inertial microfluidic-based approaches, of which vortex technology is one example.
“We think of vortex technology as a filterless filter,” says Dino Di Carlo, Ph.D., professor of bioengineering and director of the Cancer Nanotechnology Program at the Jonsson Comprehensive Cancer Center of the University of California, Los Angeles. “There aren’t any structures that are smaller than the cell types, but cells are still isolated based on size.”
Dr. Di Carlo and colleagues recently developed the High-Throughput Vortex Chip (Vortex HT), an improved microfluidic technology that allows the label-free, size-based enrichment and concentration of rare cells. The strategy involves minimal pretreatment steps, reducing cell damage, and allows an approximately 8 mL vial of blood to be processed within 15–20 minutes.
“With this approach,” asserts Dr. Di Carlo, “we can concentrate cells from any volume to about 100 µL.”
Circulating tumor cells can then be used for subsequent steps, such as real-time imaging or immunostaining. The capture efficiency, up to 83%, is slightly lower than with Dean flow fractionation and CTC-iChip, but Vortex HT generates much less contamination with white blood cells than other technologies and isolates cells in a smaller output volume.
Along with circulating tumor cells, another promising noninvasive biomarker is provided by circulating tumor DNA. Such DNA can be detected in the plasma or serum of many cancer patients as a result of the active or passive release of nucleic acid from apoptotic or necrotic tumor cells.
While circulating tumor DNA can be used to dynamically collect information about specific mutations, and provides advantages for some applications, it is not powered to offer certain types of information that can be captured only from circulating tumor cells. For example, it cannot provide details about cellular morphology or protein expression and localization. Also, it cannot enable investigators to perform proteomic profiling in parallel with genomic profiling.
These are not the only situations in which circulating DNA serves as a poor substitute for circulating tumor cells. “Another example,” notes Dr. Di Carlo, occurs with “applications that involve a drug screen that seeks to determine whether cells are sensitive or resistant to a particular compound.” Additionally, for certain cancers that have no dominant mutations, or for which mutations are not well known, circulating tumor DNA cannot provide the information that can be interrogated from profiling circulating tumor cells.
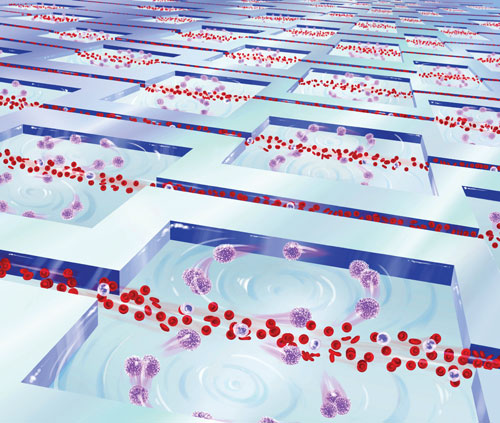
At the University of California, Los Angeles, Dino Di Carlo, Ph.D., and colleagues have developed High-Throughput Vortex Chip (Vortex-HT) technology, which uses parallel microfluidic vortex chambers to accumulate the larger circulating tumor cells from flowing blood. Vortex-HT reportedly generates less contamination with white blood cells than other technologies and isolates cells in a smaller output volume.
Insights beyond Counting
“The field started off by enumerating circulating tumor cells as a potential biomarker,” says David T. Miyamoto, M.D., Ph.D., assistant professor of radiation oncology at Harvard Medical School and the Massachusetts General Hospital (MGH). “It is currently moving toward performing detailed molecular analyses of these circulating tumor cells and using them as a form of liquid biopsy that allows us to gain insights into the molecular biology of the tumor itself.”
The Circulating Tumor Cell Center at MGH, led by Daniel Haber, M.D., Ph.D., and Mehmet Toner, Ph.D., has developed three generations of microfluidic technology. The technology of the first two generations captured circulating tumor cells on microfluidic surfaces. The technology of the third generation, known as CTC-iChip technology, introduces the unique capability—isolating cells in solution. Once the circulating tumor cells are captured or isolated, notes Dr. Miyamoto, they can be subjected to “a variety of sophisticated molecular analyses.”
In a recent study using the CTC-iChip technology, Dr. Miyamoto and colleagues performed single-cell RNA sequencing. The investigators used 77 circulating tumor cells isolated by microfluidic enrichment from 13 patients.
“The goal of this work was to use the circulating tumor cell technology to identify potential resistance mechanisms in metastatic castration-resistant prostate cancer,” explains Dr. Miyamoto. In patients who were undergoing therapy with an androgen receptor inhibitor, the retrospective analysis of their circulating tumor cells revealed that the noncanonical Wnt signaling pathway may play a role in resistance to therapy.
“We need to validate the findings in larger patient cohorts,” concludes Dr. Miyamoto. “But this proof-of-concept study shows that detailed molecular analyses of liquid biopsy samples can be used to identify potentially clinically relevant mechanisms of resistance that can then be exploited to guide patient care.”
Variable to the Last
“Most of the work on circulating tumor cells has been done in late-stage cancers to direct therapeutic interventions,” says Daniel J. O’Shannessy, Ph.D., head of translational medicine and diagnostics at Morphotek. “Even in late-stage cancers, there is a great deal of variability with respect to the numbers of cells shed for a cancer type but especially between cancer types.”
Many studies correlated the presence of circulating tumor cells with prognosis in several cancers, including breast, lung, and colorectal malignancies. However, one of the challenges associated with analyzing circulating tumor cells is that not every cancer releases them into the circulation. Also, even among cancers that do, not every cancer generates a lot of these cells.
For example, as estimated using current techniques, ovarian cancers do not appear to shed as many circulating tumor cells as several other malignancies. “Another challenge is that existing technologies are often limited by sensitivity much more than by specificity,” cautions Dr. O’Shannessy. This limitation has the potential to make interpatient comparisons, and even the longitudinal follow-up of patients, particularly difficult.
Previously, investigators at Morphotek described ApoStream®, a device that uses continuous field-flow-assist and dielectrophoresis technology to isolate and recover circulating tumor cells from the blood of cancer patients. In a recent study, Dr. O’Shannessy and colleagues used laser-scanning cytometry and highly selective antibodies to identify folate receptor alpha-positive cells from circulating tumor cells that had been isolated using the ApoStream technology.
This proof-of-principle study was able to detect folate receptor alpha-positive cells in patients with breast cancer, ovarian cancer, and non-small cell lung adenocarcinoma, but not in patients with squamous cell lung cancer. These findings supporting previous findings that were made using the respective primary or metastatic tumors.
The study demonstrated the utility of following the enrichment and identification of circulating tumor cells with immunofluorescence staining for a specific tumor marker. This combination of approaches emerges as a valuable noninvasive strategy for differentiating among tumor types. It can also be used to examine heterogeneous cell populations within tumors, particularly when tissue samples are not available.
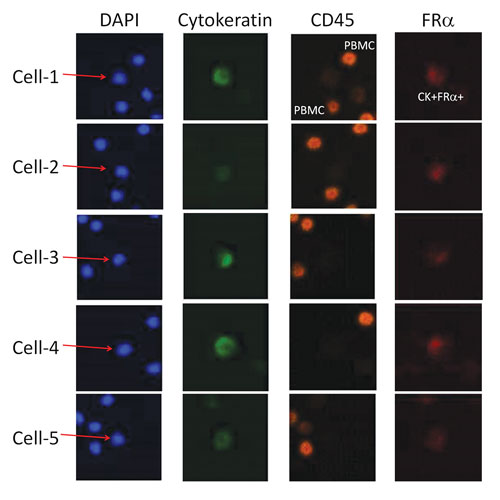
Morphotek, a biopharmaceutical company that specializes in the development of protein and antibody products through the use of gene-evolution technology, has developed the ApoStream device, which uses continuous field-flow-assist and dielectrophoresis technology to isolate and recover circulating tumor cells from the blood of cancer patients. In a recent study in Biomarker Insights, Morphotek scientists described how they interrogated ApoStream-isolated circulating tumor cells by employing laser-scanning cytometry using highly selective antibodies. The scientists detected folate receptor alpha (FRα) expression in CK+/CD45– cells isolated from lung cancer, as indicated in these representative images.
Outliers among Outliers
“We know that circulating tumor cells are present in cancer patients, but we have a limited understanding of the prognostic significance of their presence, or how to identify the ones that have more metastatic potential,” says Shana O. Kelley, Ph.D., professor of biochemistry at the University of Toronto. “These are questions we are trying to address to obtain functional information.”
Recently, Dr. Kelley and colleagues described a new molecular approach based on a fluidic chip that captures circulating tumor cells using two-dimensional sorting. At a first stage, DNA aptamers specific to cell-surface markers bound to magnetic nanoparticles are used to capture circulating tumor cells. Subsequently, at a second stage, the corresponding antisense oligonucleotides are used to release the cells, enabling two-dimensional cell sorting.
In a proof-of-concept experiment, Dr. Kelley and colleagues illustrated the strength of this approach in isolating cellular subpopulations that exhibit different phenotypes. Also, the investigators validated their results using an invasion assay.
“Progress in working on the biology of circulating tumor cells motivates us to make devices to collect information about markers much more readily,” declares Dr. Kelley. “We hope this will provide information about outcomes and prognosis.”
CTC Culturing System Reflects in Vivo Biology
New technology is making it possible for scientists to study circulating tumor cells (CTCs) from liquid biopsies without the need to amplify or enrich them. In traditional incubators, CTCs typically do not reproduce, so scientists must use amplification or enrichment methods to produce enough DNA or RNA for study, even though these methods introduce bias.
Xcell Biosciences introduced a culturing system that can reproduce cells’ native microenvironment. The system, called Avatar, is designed to maintain conditions such as oxygen and pressure levels needed for cells to proliferate as they would in vivo.
In the Avatar system, CTCs survived and propagated, according to a recent study of prostate cancer samples conducted by scientists from Xcell, Knowledge Synthesis, and the University of California, San Francisco. The study, which was presented at the recent Genitourniary Cancers Symposium, indicated that cell colonies from the same patient showed differential gene expression, a critical indication of activity from multiple tumor clones. The study also detected increased CXCR4-mediated signaling, a promising biomarker of bone metastasis.
The researchers concluded that CTCs cultured in the Avatar system accurately reflect in vivo biology, providing a tool for biomarker discovery and potentially for disease monitoring and personalized medicine.
Cancer Biomarkers Preservation in Blood
Liquid biopsy is a key tool for enabling precision medicine. For example, blood draws from patients can be obtained repeatedly for real-time monitoring of disease status and treatment efficacy through biomarkers analyses. Unfortunately, blood-borne biomarkers including circulating tumor cells (CTCs) and cell-free DNA (cfDNA) are rare and degrade rapidly upon collection.
Current stabilization technologies are limited in time of efficacy, preservation of multiple analytes, and compatibility with downstream applications, according to two scientists at Biomatrica.
To address this pre-analytics challenge, Cecille Browne, Ph.D., principal scientist, immunology hematology, and Florence Lee, Ph.D., director, liquid biopsy R&D, tapped into the company’s expertise in stabilization of biological specimens and screened the firm’s chemical library to identify CTC and cfDNA stabilizing formulations.
CTC surrogates (VCaP cells) were spiked into normal donor blood and incubated at ambient temperature for four days in the presence of EDTA, competitor or Biomatrica formulations, explained Dr. Lee, adding that Biomatrica formulations performed better than competitor formulations in white blood cells and VCaP cells recovery, VCaP-specific transcripts preservation (e.g., EpCAM and KLK3), cfDNA genomic contamination reduction, and red blood cell hemolysis inhibition.
“Preliminary testing found no interference with several downstream platforms. Biomatrica formulations could provide comprehensive alternatives to currently available blood preservatives for improved sample stability and compatibility with various downstream diagnostic platforms,” noted Dr. Lee.



