Patricia F. Fitzpatrick Dimond Ph.D. Technical Editor of Clinical OMICs President of BioInsight Communications
Finding a molecule to target each miscreant protein will take a while.
Targeting aberrant proteins by replacing them, controlling post-translational modifications that affect their function, or preventing them from interacting with their targets have proven effective approaches to disease treatment. Several companies are also seeking novel therapies that aim to fix the misfolded proteins that cause serious, currently incurable diseases.
These diseases range from neurodegenerative disorders to enzyme deficiencies. Alzheimer disease, Parkinson disease, Huntington disease, amyotrophic lateral sclerosis, and prion diseases such as Kuru and mad cow disease all involve misfolded proteins that eventually form the pathogenic aggregates characteristic of these neurodegenerative disorders. Misfolded proteins may be nonfunctional, may function suboptimally, may be easily degraded, or can expose parts of themselves leading to dysfunctional interactions with other proteins.
Little by little, a better understanding of the mechanisms that drive protein interactions and some definition of the states in which proteins become pathogenic is emerging. Two quality control systems that operate in cells ensure accuracy of protein folding. A chaperone system prevents the aggregation of partially folded proteins and facilitates complete folding. The second is a sort of protein garbage disposal system that identifies and degrades improperly folded and damaged proteins.
Proteins are also the ultimate moving targets for potential therapeutics. Under normal physiological conditions, native proteins don’t adopt a single static conformation. Rather, a protein’s true native state includes small fluctuations around the native conformation, partially unfolded forms, and even globally unfolded forms.
Leveraging the Garbage-Disposal System
Basic scientists and drug development companies are chasing misfolded proteins down several cellular paths. A nonspecific approach involves ridding the cell of toxic proteins by taping into the cell’s waste-management system. Cells create and discard proteins continuously, a process that relies on a balance between how quickly proteins are created and damaged ones destroyed.
To achieve the balance, cells use proteasomes, protein-degrading enzyme complexes consisting of multiple subunits that exist in the cell nucleus and cytoplasm. Protein destruction occurs by marking proteins for disposal by tagging them with ubiquitin, a small protein that latches onto the proteins, often forming long chains.
The proteasome then recognizes these ubiquitinated proteins and breaks them down. Attachment of one single ubiquitin molecule to a protein signals other ligase enzymes to attach additional ubiquitin molecules. The result is a polyubiquitin chain that is bound by the proteasome, allowing it to degrade the tagged protein.
Harvard University researchers reported results on a study that focused on proteasome activity in the September 2010 issue of Nature. Their work was funded by the Harvard Technology Development Accelerator Fund, Johnson & Johnson, Merck & Co., and NIH.
They found that when the ligase Usp14 is activated, it interrupts the ubiquitin chain, thereby slowing the proteasome’s ability to rid the cell of undesirable proteins. As a result the cell makes new proteins faster than it rids itself of the old ones, leading to a buildup of misfolded proteins.
The investigators then screened 63,000 compounds and reportedly identified a Usp14 inhibitor, IU1, that when added to cells increased proteasome activity apparently due to its ability to trim the ubiquitin tail. As of September 2010, patents were pending for IU1 and the assay used to identify the molecule.
Using Chaperones
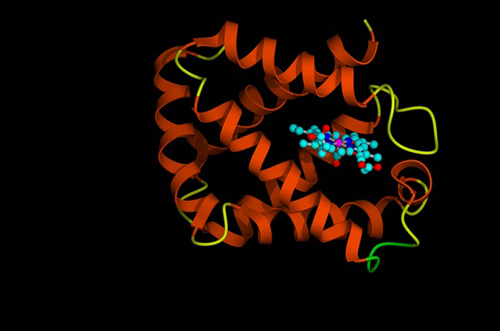
Amicus Therapeutics approaches treatment of human genetic diseases by using its pharmacological chaperones, or small molecule drugs that selectively bind to the target protein. Once bound, these molecules increase the protein’s stability and encourage it to fold into the correct 3-D shape.
Amicus’ lead candidate is in Phase III trials to treat Fabry disease. The company, along with partner GlaxoSmithKline (GSK), is conducting a Phase III study and expects preliminary results in mid-2011. In February Amicus announced positive data from its ongoing Phase II extension study. Fifteen subjects have been treated for more than three years, seven subjects have been treated for more than four years, and 17 continue to receive treatment in the ongoing extension study.
Renal function is a key efficacy endpoint for Fabry disease treatments. The trial showed that estimated glomerular filtration rate, a measure of kidney function, remained stable out to 3–4 years for all subjects continuing in the extension study. Reduced 24-hour urine protein levels, another measure of renal function, was observed with a mean 21% and median 34% reduction from baseline in patients identified as responders.
Apart from GSK, another big pharma company made a major commitment in the protein folding space. Pfizer acquired FoldRx Pharmaceuticals in September 2010 for its pipeline of preclinical and clinical products to treat diseases caused by protein misfolding. Lead product, tafamidis, is being developed for TTR amyloidosis, a disease linked to mutations in the transthyretin (TTR) protein.
TTR amyloidosis manifests in two clinical forms: ATTR-PN, a sensory neuropathy that starts in the lower extremities and progresses to include both autonomic and motor dysfunction, and ATTR-CM, characterized by amyloid deposits that infiltrate the heart and result in a potential fatal restrictive cardiomyopathy. ATTR-CM generally occurs in individuals over 60 years of age. ATTR-PN affects about 5,000–10,000 patients worldwide, while ATTR-CM affects about 400,000 patients in the U.S alone.
Tafamidis works to prevent the dissociation of native TTR tetramer into monomers. This results in the inhibition of amyloid fibril formation that leads to amyloid deposition. The last report on clinical investigations was made in 2009. FoldRx said preliminary results from the first randomized, controlled trial showed that treatment significantly halted disease progression in ATTR-PN, reduced the burden of disease after 18 months, and appeared to be safe and well-tolerated.
Pfizer has filed an MAA and is currently in communication with the FDA to define its path for filing in the U.S. Tafamidis has orphan drug designation in both the U.S. and EU as well as Fast Track designation in the U.S. for the treatment of ATTR-PN.
The Protein Homeostasis
Proteostasis Therapeutics is working to discover small molecules that restore protein folding, trafficking, and clearance pathways and is developing them as drugs for neurodegenerative and orphan diseases. Together, these pathways make up the protein homeostasis (proteostasis) network. Founded in 2008 to develop Proteostasis Regulator™ drugs, the company raised $45 million in a 2010 Series A financing.
Peter Reinhart, Ph.D., the company’s president and CSO, defined proteostasis as a “recent concept that brings together a number of pathways and protein complexes that have previously been viewed separately without the emergent understanding that comes from the realization that they form an interconnected network. The proteostasis network, composed of about 1,000 proteins, contains the ubiquitin proteasome system, chaperones, membrane trafficking pathways, and autophagy.
“It is the cellular machinery positioned between the birth of a new polypeptide chain and the protein’s final conformation, helping to maintain the folded protein at the correct location and at the appropriate concentration for all of its interactions and functions.” The functionality of the proteostasis network is compromised by cellular stress and declines with age.
Dr. Reinhart says that the company studies the proteostasis network in its entirety, focusing on 10 to 12 different pathways, to build network signatures that define disease progression. “We are getting these signatures by focusing on specific target diseases like cystic fibrosis and Huntington, Parkinson, and Alzheimer diseases.
“We collect high-quality, well-annotated human postmortem tissues to analyze how the proteostasis network is altered during disease progression. We can then find pathways and individual proteins that change early in the disease as well as others that change much later during disease progression, providing us a very dynamic view of the changing capability of cells to fold and traffic proteins or remove misfolded and aggregated proteins.”
As progress continues toward fixing misfolded proteins the question remains whether each misfolded protein will require its own specific therapeutic or whether a global, network-focused approach will be needed. Either approach, however, may provide some hope for treating previously intractable human diseases. While a fertile field for drug discovery, finding each miscreant protein form and a molecule to target it will take a while.
Patricia F. Dimond, Ph.D. ([email protected]), is a principal at BioInsight Consulting.