Scientists at the Icahn School of Medicine at Mount Sinai and colleagues say they have harnessed the power of machine learning to identify key predictors of mortality in dementia patients. Their study “Machine learning models identify predictive features of patient mortality across dementia types,” published online in Communications Medicine, addresses on critical challenges in dementia care by pinpointing patients at high risk of near-term death and reportedly uncovers the factors that drive this risk.
Unlike previous studies that focused on diagnosing dementia, this research delves into predicting patient prognosis, shedding light on mortality risks, and contributing factors in various kinds of dementia.
Major cause of death
Dementia has emerged as a major cause of death in societies with increasingly aging populations. However, predicting the exact timing of death in dementia cases is challenging due to the variable progression of cognitive decline affecting the body’s normal functions, say the researchers.
“We developed machine-learning models predicting dementia patient mortality at four different survival thresholds using a dataset of 45,275 unique participants and 163,782 visit records from the U.S. National Alzheimer’s Coordinating Center (NACC). We built multi-factorial XGBoost models using a small set of mortality predictors and conducted stratified analyses with dementia type-specific models,” write the investigators.
“Our models achieved an area under the receiver operating characteristic curve (AUC-ROC) of over 0.82 utilizing nine parsimonious features for all 1-, 3-, 5-, and 10-year thresholds. The trained models mainly consisted of dementia-related predictors such as specific neuropsychological tests and were minimally affected by other age-related causes of death, e.g., stroke and cardiovascular conditions.
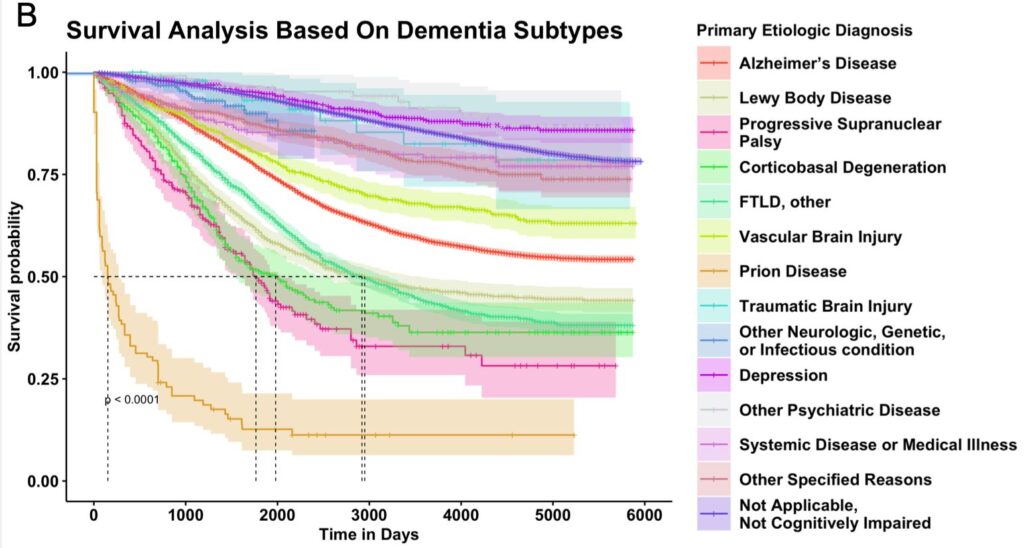
“Notably, stratified analyses revealed shared and distinct predictors of mortality across eight dementia types. Unsupervised clustering of mortality predictors grouped vascular dementia with depression and Lewy body dementia with frontotemporal lobar dementia.
“This study demonstrates the feasibility of flagging dementia patients at risk of mortality for personalized clinical management. Parsimonious machine-learning models can be used to predict dementia patient mortality with a limited set of clinical features, and dementia type-specific models can be applied to heterogeneous dementia patient populations.”
“Our findings are significant as they illustrate the potential of machine learning models to accurately anticipate mortality risk in dementia patients over varying timeframes,” said corresponding author Kuan-lin Huang, PhD, assistant professor of genetics and genomic sciences at Icahn Mount Sinai. “By pinpointing a concise set of clinical features, including performance on neuropsychological and other available testing, our models empower health care providers to make more informed decisions about patient care, potentially leading to more tailored and timely interventions.”
The study also found that neuropsychological test results were a better predictor of mortality risk in dementia patients than age-related factors such as cancer and heart disease, underscoring dementia’s significant role in mortality among those with neurodegenerative conditions.
“The implications of our research extend beyond clinical practice, as it underscores the value of machine learning in unraveling the complexities of diseases like dementia,” continued Huang.
“This study lays the groundwork for future investigations into predictive modeling in dementia care. However, while machine learning holds great promise for improving dementia care, it’s important to remember that these models aren’t crystal balls for individual outcomes. Many factors, both personal and medical, shape a patient’s journey.”
Next, the research team plans to refine their models by incorporating treatment effects and genetic data and exploring advanced deep-learning techniques for even more precise predictions.
Given the aging population, dementia has emerged as an increasingly pressing public health concern, ranking as the seventh leading cause of death and the fourth most burdensome disease or injury in the United States in 2016, based on years of life lost. As of 2022, Alzheimer’s and other dementias cost an estimated $1 trillion annually, impacting approximately 6.5 million Americans and 57.4 million people worldwide, with projections suggesting a tripling by 2050.



