![CRISPR technology has been used to rewire the genetic circuits of stem cells to produce an anti-inflammatory arthritis drug when the cells encounter inflammation. The technique eventually could act as a vaccine for arthritis and other chronic conditions. [Ella Marushchenko]](https://genengnews.com/wp-content/uploads/2018/08/Apr28_2017_EllaMarushchenko_StemCellAntiInflammatoryDrug1061646167-1.jpg)
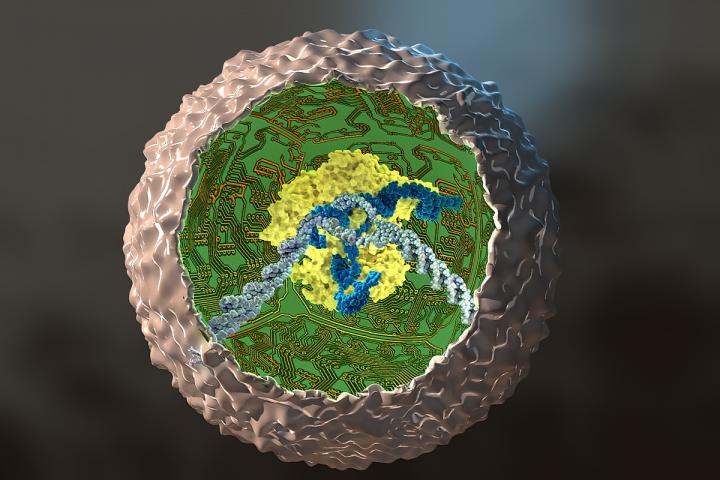
CRISPR technology has been used to rewire the genetic circuits of stem cells to produce an anti-inflammatory arthritis drug when the cells encounter inflammation. The technique eventually could act as a vaccine for arthritis and other chronic conditions. [Ella Marushchenko]
We have anti-arthritis drugs. What we lack is the ability to deploy them when and where they are needed in the body. The drugs would be far more effective, and occasion fewer side effects, if they were to appear only in response to inflammation, and only in the joints. If the drugs could be delivered so painstakingly—so smartly—they wouldn’t have to be administered systemically.
Although conventional drug delivery systems may be unable to respond to arthritic flares with such adroitness, cells may have better luck—if they are suitably modified. Stem cells, for example, have been “rewired” by means of gene-editing technology to fight arthritis. These stem cells, known as SMART cells (Stem cells Modified for Autonomous Regenerative Therapy), develop into cartilage cells that produce a biologic anti-inflammatory drug. Ideally, the new cartilage cells will replace arthritic cartilage, and the biologic will protect against chronic inflammation, preserving joints and other tissues.
SMART cells of this sort were prepared by scientists based at Washington University School of Medicine in St. Louis. The scientists initially worked with skin cells taken from the tails of mice and converted those cells into stem cells. Then, using the gene-editing tool CRISPR in cells grown in culture, they removed a key gene in the inflammatory process and replaced it with a gene that releases a biologic drug that combats inflammation.
Details of this work appeared April 27 in the journal Stem Cell Reports, in an article entitled “Genome Engineering of Stem Cells for Autonomously Regulated, Closed-Loop Delivery of Biologic Drugs.” The article describes how modified stem cells grew into cartilage and produced cartilage tissue. The engineered cartilage, the scientists reported, was protected from inflammation.
“Using the CRISPR/Cas9 genome-engineering system, we created stem cells that antagonize IL-1- [interleukin-1] or TNF-α- [tumor necrosis factor-α] mediated inflammation in an autoregulated, feedback-controlled manner,” wrote the authors of the Stem Cell Reports article. “Our results show that genome engineering can be used successfully to rewire endogenous cell circuits to allow for prescribed input/output relationships between inflammatory mediators and their antagonists, providing a foundation for cell-based drug delivery or cell-based vaccines via a rapidly responsive, autoregulated system.”
Many current drugs used to treat arthritis—including Enbrel® (etanercept), Humira® (adalimumab), and Remicade® (infliximab)—attack TNF-α, an inflammation-promoting molecule. But the problem with these drugs is that they are given systemically rather than targeted to joints. As a result, they interfere with the immune system throughout the body and can make patients susceptible to side effects such as infections.
“We want to use our gene-editing technology as a way to deliver targeted therapy in response to localized inflammation in a joint, as opposed to current drug therapies that can interfere with the inflammatory response through the entire body,” said Farshid Guilak, Ph.D., the paper's senior author and a professor of orthopedic surgery at Washington University School of Medicine. “If this strategy proves to be successful, the engineered cells only would block inflammation when inflammatory signals are released, such as during an arthritic flare in that joint.”
Dr. Guilak's team encoded the stem/cartilage cells with genes that made the cells light up when responding to inflammation, so the scientists easily could determine when the cells were responding. Recently, the team began testing the engineered stem cells in mouse models of rheumatoid arthritis and other inflammatory diseases.
If the work can be replicated in animals and then developed into a clinical therapy, the engineered cells or cartilage grown from stem cells would respond to inflammation by releasing a biologic drug—the TNF-α inhibitor—that would protect the synthetic cartilage cells that Dr. Guilak's team created and the natural cartilage cells in specific joints.
“When these cells see TNF-α, they rapidly activate a therapy that reduces inflammation,” Dr. Guilak explained. “We believe this strategy also may work for other systems that depend on a feedback loop. In diabetes, for example, it's possible we could make stem cells that would sense glucose and turn on insulin in response. We are using pluripotent stem cells, so we can make them into any cell type, and with CRISPR, we can remove or insert genes that have the potential to treat many types of disorders.”