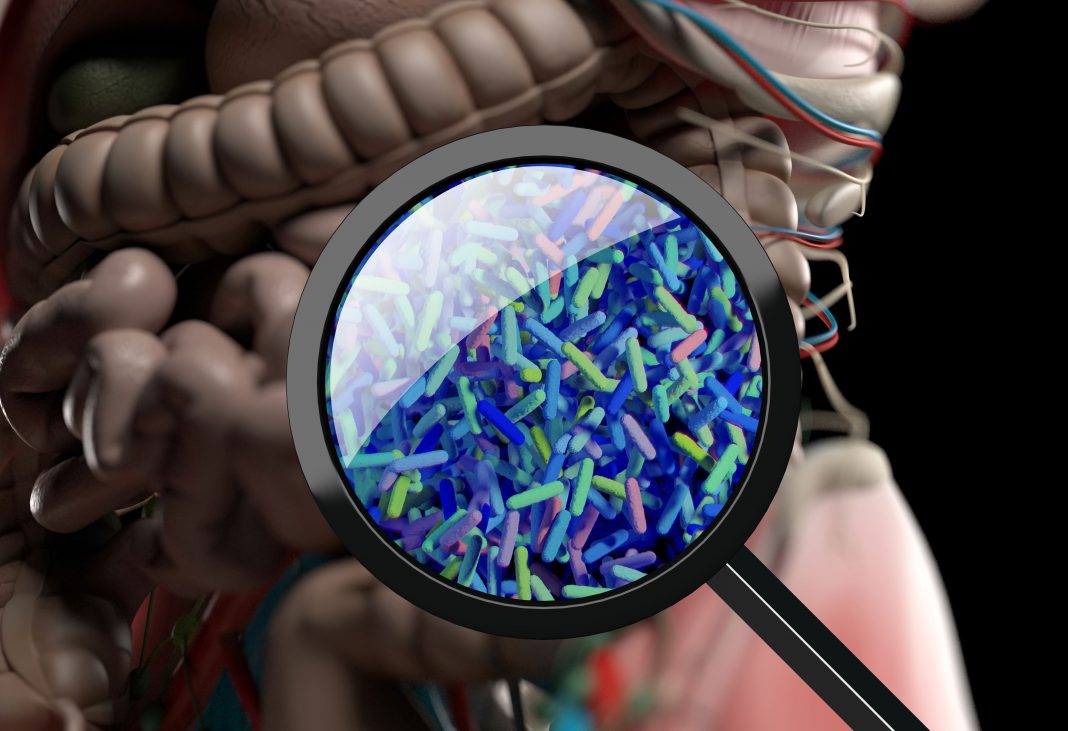
Researchers from North Carolina State University (NC State), the University of North Carolina (UNC) at Chapel Hill, and the University of California, San Diego, report they have discovered that enzymes within a class known as bile salt hydrolases (BSHs) can restrict Clostridioides difficile (C. diff.) colonization by both altering existing bile acids and by creating a new class of bile acids within the gut’s microbial environment. The work could lead to “designer” probiotics that protect against disease by introducing specific BSHs to the gut after antibiotic treatment.
The findings are published in Nature Microbiology in an article titled, “Bile salt hydrolases shape the bile acid landscape and restrict C. difficile growth in the murine gut.”
Although researchers had long suspected a connection between BSHs from beneficial bacteria, the bile acid pool, gut microbial composition, and host health, little was known about how BSHs function and their potential impacts on host health.
“The old dogma—that BSHs are needed for gut colonization because they render toxic bile acids nontoxic—oversimplified what’s actually happening,” said Casey Theriot, PhD, associate professor of infectious disease at North Carolina State University and co-corresponding author of the study.
“The reality is that BSHs’ interactions are context-dependent, meaning they’re affected by the type of bacteria they come from,” Theriot said. “And they don’t just interact with bile acids produced by the host. BSHs in the microbiota can create and interact with a new class of bile acids called microbial conjugated bile acids (MCBAs)—bile acids that we didn’t even know existed until recently.”
The researchers looked at hundreds of BSHs from different Lactobacillaceae bacteria and then included BSHs from the gut microbiota.
“We found the tiny molecular fingerprint that defined whether a BSH would ‘turn left’ or ‘turn right’ in terms of what they processed,” said Matthew Redinbo, PhD, the Kenan distinguished professor of chemistry in UNC-Chapel Hill’s College of Arts and Sciences. “Knowing that allowed Casey’s team to steer the bile acid pool in whatever direction they wanted.”
The researchers used a cocktail of Lactobacillus BSHs to figure out if they could change the bile acid pool enough to alter C. diff colonization in both human stool samples collected from patients susceptible to C. diff infection (CDI) and in a mouse model of CDI. In both human stool samples and mice, the researchers saw that pre-treatment with BSH cocktails impacted C. diff colonization. Interestingly, the researchers noted elevated levels of MCBAs in the gut microbiota of the BSH-treated mice.
To determine whether the MCBAs were also involved in inhibiting C. diff germination and growth, they tested the MCBAs against C. diff in vitro. In most cases, the presence of MCBAs inhibited multiple steps of the C. diff life cycle.
“This is more evidence that BSHs are driving changes in the bile acid pool—including making MCBAs—that could serve to inhibit C. diff,” Theriot said. “We’ve uncovered a new function for BSH enzymes.”
“This work highlights the importance of BSHs as key intestinal enzymes and promising new therapeutics,” said Matt Foley, PhD, research scholar at NC State and co-first author of the study. “Using BSHs in combination with other strategies may offer a new approach to treat C. diff.”
The research may lead to potential probiotics that could be customized to protect against a variety of bacterial infections and intestinal diseases.
“This is an important illustration of how deciphering the biochemical and genetic basis for probiotic functionality both leads to a better understanding of how we can combat gut disease with novel modalities, and also practically design and formulate next-generation commercial probiotics,” said Rodolphe Barrangou, PhD, the Todd R. Klaenhammer distinguished professor in probiotics research at NC State and co-corresponding author of the study.