![Transmission electron micrograph of the Sin Nombre virus, a virulent species of hantavirus. [CDC/ Cynthia Goldsmith, Luanne Elliott]](https://genengnews.com/wp-content/uploads/2018/08/1137_lores2134918255-1.jpg)
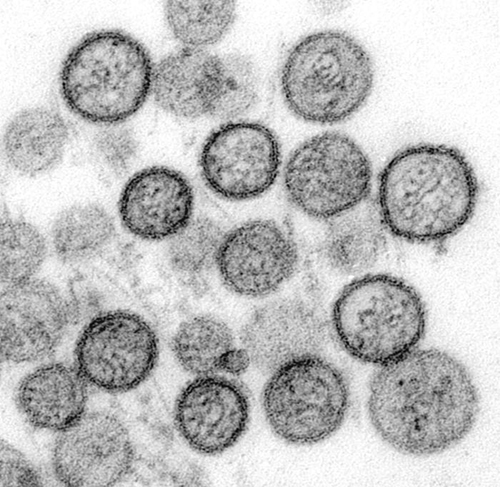
Transmission electron micrograph of the Sin Nombre virus, a virulent species of hantavirus. [CDC/ Cynthia Goldsmith, Luanne Elliott]
Understanding how infectious agents hijack host factors to gain entry into cells is of paramount importance for an array of contagious diseases. In particular, hantavirus, the causative agent of a hemorrhagic fever with severe renal or pulmonary symptoms, has recently been shown to have a unique method of host cell entry.
Researchers from the Albert Einstein College of Medicine and U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) have discovered that hantaviruses use cholesterol molecules contained within cell membranes to gain access into cells and infect humans.
“Our work demonstrates that hantaviruses are extremely sensitive to the amount of cholesterol in the membranes of the cells they are trying to infect,” explained senior author Kartik Chandran, Ph.D., associate professor of microbiology and immunology at the Albert Einstein College of Medicine. “Cholesterol seems to control the ability of hantaviruses to fuse with cell membranes and get inside, into the cytoplasm, which is where all the goodies are to make more virus.”
The findings from this study were published recently in mBio through an article entitled “Haploid Genetic Screen Reveals a Profound and Direct Dependence on Cholesterol for Hantavirus Membrane Fusion.”
Hantaviruses typically affect rodents, but can be transferred to humans through contact with the rodent’s urine, saliva, or droppings. Hantavirus strains in Europe and Asia have caused hemorrhagic fever with kidney failure while strains in the Americas have caused hantavirus cardiopulmonary syndrome, a severe and often fatal respiratory disease.
Utilizing isolated human cells, the investigators of the current study performed a genetic screen to identify host factors required for viral entry. They found that multiple genes involved in cholesterol sensing, regulation, and biosynthesis, including key components of the sterol response element-binding protein (SREBP) pathway, were critical for hantavirus to gain access to the host cell cytoplasm.
The scientists were able to fuse the gene encoding the hantavirus entry machinery into a normally innocuous virus, in order to study its ability to attack isolated human cells. Interestingly, the researchers found that if they disrupted the membrane-bound transcription factor peptidase/site-1 protease (MBTPS1/S1P), which is an SREBP control element, using either genetic or pharmacologic methods they were able to dramatically reduce infection by the engineered virus, as well as wild-type virulent hantavirus strains.
“It is conceivable that cholesterol-lowering drugs could lead to treatments for hantavirus infection,” stated co-senior author John M. Dye, Jr., Ph.D., viral immunology branch chief at USAMRIID. “However, such drugs would need to reduce cholesterol levels in key hantavirus target tissues in a human, whereas typical cholesterol-lowering drugs like statins target primarily the liver. It remains to be seen if this can be done safely.”
The research teams were excited by their findings, but admit that additional studies are required to better understand why hantaviruses are seemingly so dependent on cholesterol, and if that mechanism has evolved in other viruses of the same family.