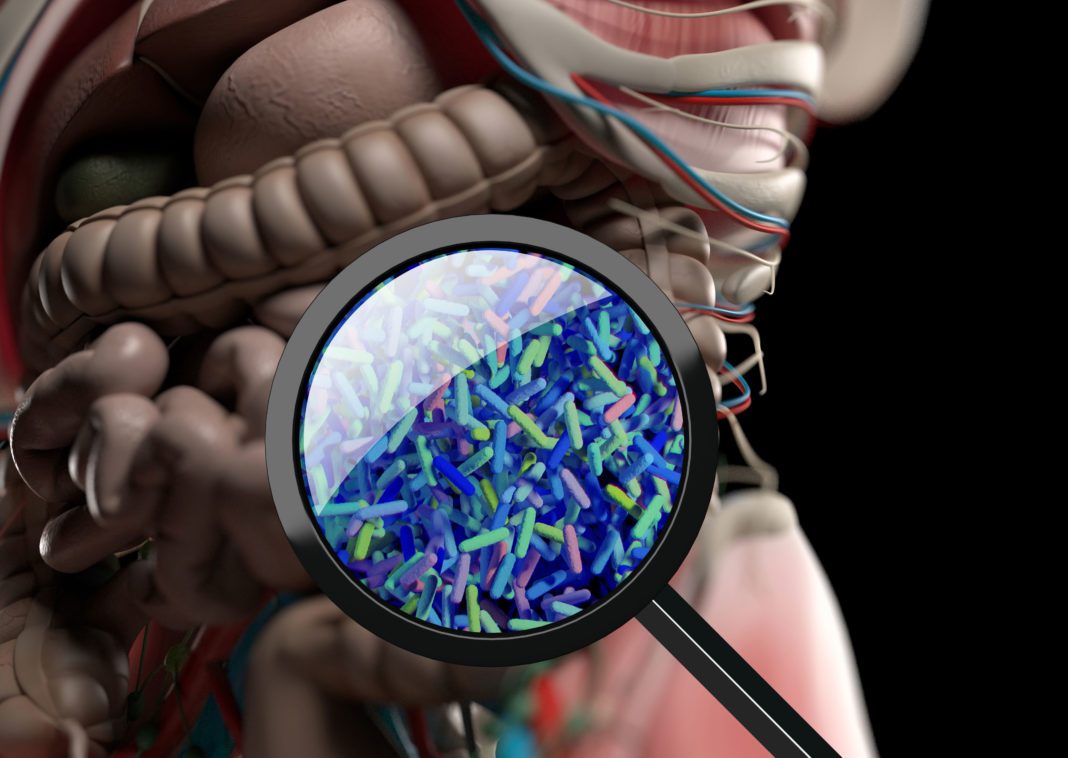
A new study in mice exploring the gut-skin axis has demonstrated that microbial fermentation of dietary fiber in the gut can protect against allergic skin disease. The findings could potentially lead to novel treatments to prevent or treat allergies.
Researchers from Monash University collaborated with researchers at the University Hospital of Lausanne (CHUV) and demonstrated how the fermentation of fiber in the gut by bacteria and subsequent production of short-chain fatty acids (SCFAs), specifically butyrate, protected against atopic dermatitis (AD) in mice.
The research was published in Mucosal Immunology in a paper titled, “Gut-derived short-chain fatty acids modulate skin barrier integrity by promoting keratinocyte metabolism and differentiation,” and led by professor Ben Marsland, PhD, professor at the Central Clinical School’s department of immunology at Monash University.
“Barrier integrity is central to the maintenance of healthy immunological homeostasis,” wrote the researchers. “Impaired skin barrier function is linked with enhanced allergen sensitization and the development of diseases such as AD, which can precede the development of other allergic disorders, for example, food allergies and asthma.”
“Previous work from our group, and others, has focused on the local health benefits of SCFAs in the gut as well as at distal sites such as the lung and cardiovascular system,” Marsland said. “We wondered if this might also extend to the skin, which is an area that has not really been investigated.
The scientists fed mice a diet high in fermentable fiber or gave them purified SCFAs. “This treatment was profoundly protective against allergic skin inflammation,” Marsland said.
“The upshot of this was that the skin barrier was fortified against allergens—we were using house dust mite allergens—that would normally penetrate the skin barrier, activate the immune system, and start an allergic reaction in these models,” Marsland explained.
“It turns out the immune system was secondary to this skin barrier function.”
SCFAs could be administered orally or directly on the skin as a cream, bypassing the gut, he added.
“Using an experimental model of AD-like skin inflammation, we report that a fermentable fiber-rich diet alleviates systemic allergen sensitization and disease severity,” added the researchers. “The gut-skin axis underpins this phenomenon through SCFA production, particularly butyrate, which strengthens skin barrier function by altering mitochondrial metabolism of epidermal keratinocytes and the production of key structural components.”
Their results demonstrate that dietary fiber and SCFA improve epidermal barrier integrity, ultimately limiting early allergen sensitization and disease development.