Studies in mice by researchers at the University of Melbourne and Monash University, have uncovered a mechanistic link between stress and weakened immunity. Their studies found under conditions of stress the neurotransmitter noradrenaline (NA)—which plays a key role in the fight-or-flight stress response—impairs immune responses by inhibiting the movements of various white blood cells in different tissues. Experiments in mice showed that this fast and transient inhibitory effect on immune cell motility occurred in animals with infections and with cancer. It’s not yet clear whether the findings will generalize to humans with various health conditions.
“We found that stress can cause immune cells to stop moving and prevents immune cells from protecting against disease,” said the University of Melbourne’s author Scott Mueller, PhD, of the Peter Doherty Institute for Infection and Immunity (Doherty Institute). “This is novel because it was not known that stress signals can stop immune cells from moving about in the body and performing their job … This knowledge will allow us to test the impact of drugs that block the sympathetic stress pathway, such as beta blockers, on the outcomes of vaccination and cancer treatments. These types of drugs might be safe treatment options for patients where stress could contribute to poor immune function.”
Senior study author Mueller, and colleagues report their work in Immunity, in a paper titled, “Adrenergic regulation of the vasculature impairs leukocyte interstitial migration and suppresses immune responses.”
A primary function of the sympathetic nervous system (SNS) is to control diverse biological processes, such as heart rate and blood flow, which prepare the body to fight or take flight in stressful or dangerous situations. “Most tissues, including the lymph nodes (LNs) and spleen, are innervated by SNS fibers, and highly diverse cell types respond to SNS neurotransmitters through cell surface G protein-coupled α- or β-adrenergic receptors (ARs),” the authors wrote.
Stress-induced activation of the SNS can suppress immune responses in various ways, but the underlying mechanisms have been poorly characterized. “We hypothesized that SNS signals might modify the movement of T cells in tissues and lead to compromised immunity,” Mueller noted.
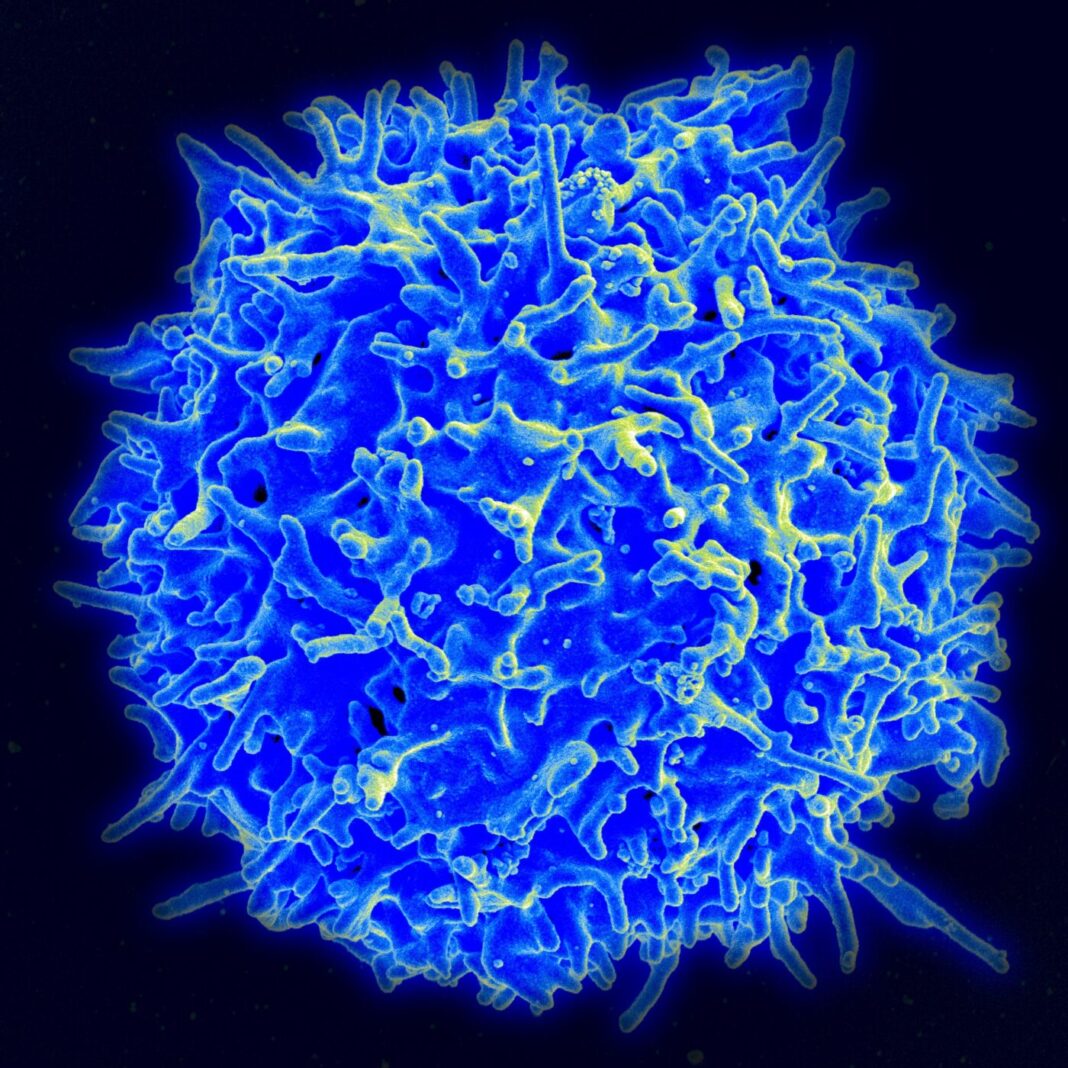
Leukocytes—white blood cells—travel constantly throughout the body and are highly motile within tissues, where they locate and eradicate pathogens and tumors. “The motility of leukocytes is therefore critical for immunity,” the authors commented. But while the movement of leukocytes is vital for immunity, it’s not clear how these cells integrate various signals to navigate within tissues.
Immune cell movement is affected by the physical microenvironment, as well as by different types of signal, including adhesion and chemotactic factors, metabolites, and tissue oxygenation, the authors noted. “Leukocytes integrate these signals to make rapid decisions
that control cell behavior.” It’s thus possible that activation of neural signaling and the release of neurotransmitters might affect the motility and behavior of leukocytes as they navigate within tissues. “ … neurotransmitter signals might be a rapid way to modulate leukocyte behavior in tissues, in particular during acute stress that involves increased activation of the SNS,” the team continued. As Mueller stated, “We also speculated that neurotransmitter signals might be a rapid way to modulate leukocyte behavior in tissues, in particular during acute stress that involves increased activation of the SNS.” Mueller said.
To test this idea, the researchers used advanced imaging to track the movements of T cells in mouse lymph nodes. They found that within minutes of being exposed to noradrenaline, T cells that had been rapidly moving stopped in their tracks and retracted their arm-like protrusions. This effect was transient, lasting between 45 and 60 minutes. Localized administration of noradrenaline in the lymph nodes of live mice also rapidly halted the cells. Similar effects were observed in mice that received noradrenaline infusions, which are used to treat patients with septic shock—a life-threatening condition that occurs when infection leads to dangerously low blood pressure. This finding suggests that therapeutic treatment with noradrenaline might impair leukocyte functions.
“We were very surprised that stress signals had such a rapid and dramatic effect on how immune cells move,” Mueller stated. “Since movement is central to how immune cells can get to the right parts of the body and fight infections or tumors, this rapid movement off-switch was unexpected.”

“Our results reveal that an unanticipated consequence of modulation of blood flow in response to SNS activity is the rapid sensing of changes in oxygen by leukocytes and the inhibition of motility,” Mueller explained. “Such rapid paralysis of leukocyte behavior identifies a physiological consequence of SNS activity that explains at least in part the widely observed relationship between stress and impaired immunity,” the authors added.
Their study results demonstrated that SNS signals impaired protective immunity against pathogens and tumors in various mouse models, decreasing the proliferation and expansion of T cells in the lymph nodes and spleen. For example, treatment with SNS-stimulating molecules rapidly stopped the movements of T cells and dendritic cells in mice infected with herpes simplex virus 1 and reduced virus-specific T cell recruitment to the site of the skin infection. Similar effects were observed in mice with melanoma and in mice infected with a malarial parasite. “These findings provide mechanistic insight into the relationship between activation of ARs and impaired immunity,” the team wrote.
However, they acknowledged, “To what degree different signals that activate the SNS can drive local changes to tissue blood flow and affect leukocyte behavior remains to be determined in humans.”
The findings point to the possibility that increased SNS activity, particularly in individuals with underlying health conditions, might result in impaired leukocyte behavior and function. The results could thus have important health implications for patients who use SNS-activating drugs to treat diseases such as heart failure, sepsis, asthma, and allergic reactions. “Notably, increased SNS activity is prominent in patients with obesity and heart failure, while acute psychological stress can cause vasoconstriction in patients with heart disease, the scientists noted. “The finding that SNS activity regulated tissue hypoxia may have implications for anti-tumor immunity and the effectiveness of immunotherapies … It will be critical to further evaluate the effect of sympathomimetic drug use on immune outcomes in patients, as well as the potential for therapeutic intervention of this pathway.”
Mueller concluded, “Our data suggest that SNS activity in tissues could impact immune outcomes in diverse diseases. Further insight into the impact of adrenergic receptor signals on cellular functions in tissues may inform the development of improved treatments for infections and cancer.”