New therapeutics must clear many hurdles before they are approved for use in the general population. Clinical trials play an essential role in that journey, but the important knowledge gained before a compound makes it to a clinical trial has become increasingly significant. As has been seen in many cases, success in the clinic is built upon preclinical knowledge. Greater success in the clinic, then, could be achieved if drug development were to find ways to improve preclinical knowledge. One way to improve preclinical knowledge is to use disease model platforms, such as 3D organoids, that can more closely mimic human tissues and support disease models that can intensify the study and manipulation of pathophysiology.
Improving preclinical knowledge
There is a significant need to understand the efficacy of a compound earlier in research and discovery. Doing so would allow ineffective compounds to be rejected sooner in the overall process. Currently, most drugs are validated in simplistic 2D systems of cultured cells comprised of one cell type. The simplicity fails to replicate the complex and multidimensional nature of human systems, where various cells inherently interact with each other and the extracellular matrix.
Organoids, derived from a patient’s actual stem cells, recreate the complexity of human tissue and allow models to be developed that represent the complexity of human disease. Comprised of many cell types, organoids better recapitulate disease biology outside of the human body. They can provide a greater understanding of a drug’s potential efficacy and adverse effects earlier in the research process.
“Phase 0” studies are a new and promising approach in clinical trials. Ordinarily, they involve the administration of microdoses of candidate drugs to small patient populations, and they are designed to yield pharmacokinetic information. However, Phase 0 studies may also involve the use of multidimensional disease models that are based on human organoids, or “organs in a dish.” Such models may yield information suggestive of a drug’s safety and efficacy.
Organoid models that mimic in vivo human physiology, while representing an individual’s own genotype and phenotype, have in- credible potential to offer a better picture of what researchers might see when a drug is brought into the clinic in specific patient populations, making treatment choices much more personalized.
Further, an earlier understanding of a drug’s clinical profile, toxicity, and efficacy can have implications for pricing and timing. By identifying unsuccessful compounds earlier in the process, researchers can spend more time on compounds with greater potential, possibly bringing therapies to patients faster and at a lower price point.
“Gut in a dish” for developing personalized therapies
Expanding upon the organ-in-a-dish technology, the gut-in-a-dish platform is designed to mimic the physiological state of the gut, and to support models that recreate disease-specific changes that take place on cellular and extracellular levels. Reverse-engineered gut organoids comprise epithelial cells, immune cells, and microbes and allow the investigation of mechanisms for gastrointestinal inflammatory diseases, both neoplastic and non-neoplastic.
A gut-in-a-dish that captures the complexity of the gut mucosa, either mouse or human, is created by collecting biopsy specimens (from healthy or disease subjects) from which stem cells are isolated, embedded in Corning® Matrigel® matrix, and differentiated into enteroid-derived monolayers (EDMs) in Transwell®-permeable supports, creating “personalized” 3D organoids.
Matrigel matrix has been the gold standard for organoid cultures, as it provides the necessary physiological milieu to support 3D structures. By offering an extracellular matrix (ECM) specifically for culturing organoids, Matrigel matrix helps reduce some of the inherent variability in these types of workflows.1,2 In fact, each lot has a specific elastic modulus value indicating the stiffness of the gel formed and is qualified to form stable 3D domes, commonly used in organoid culture protocols such as those for gut-in-a-dish models.
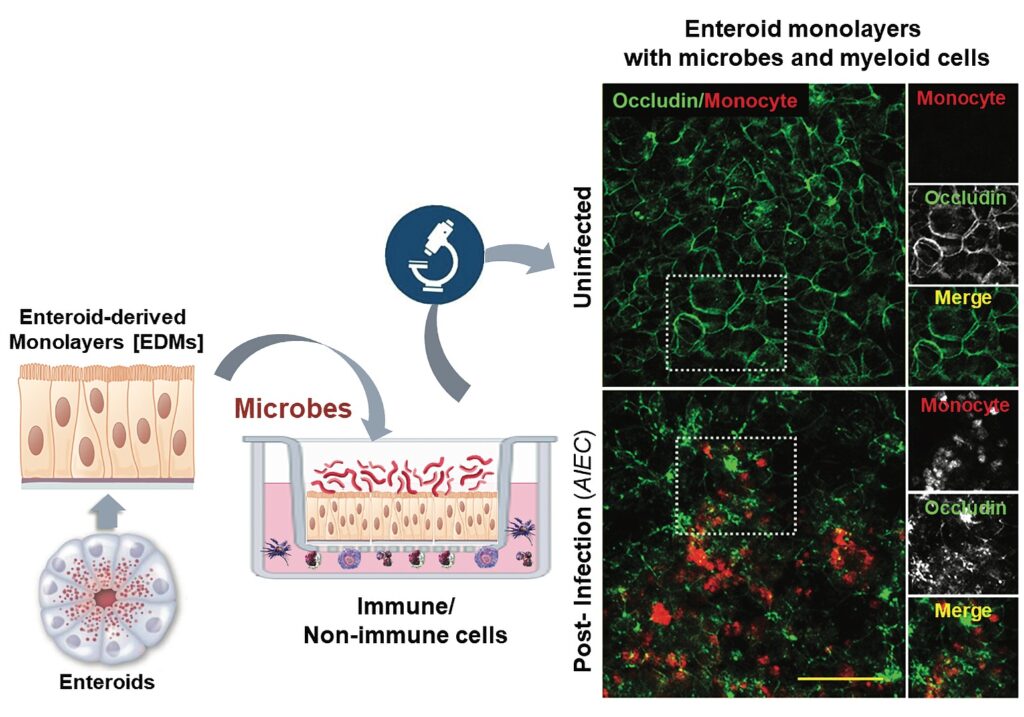
Various processes, pathways, and targets can be identified and studied when disease models built on the gut-in-a-dish platform are manipulated. For example, the interaction of microbes, epithelial cells, and immune cells can be examined to further the understand-
ing of inflammatory bowel disease mechanisms and identify early biomarkers that can be targeted.3,4 The model can also be used to validate targets by disrupting or activating the respective pathways and observing the effect within the model (including Phase 0 drug testing).5 Further insight can be gained by looking at effect versus patients or population characteristics, potentially opening the door for developing personalized therapies based on phenotype and genotype.
The success of these preclinical efforts rests heavily on the available tools that enable ex vivo modeling to mirror the in vivo environment. Complex 3D systems such as the gut-in-a-dish platform require advanced and reliable culture tools. Growth media and culture conditions must be carefully considered when dealing with a complex system. In this example, the system relies on the Matrigel matrix—a gelatinous protein mixture that contains several proteins, carbohydrates, and growth factors. With over 10,000 citations, it is the most frequently used extracellular matrix for organoid formation.6
To bring this technology to fruition at a larger scale, one that would allow for preclinical application, the technology must be adapted to a high-throughput screening model. This screening has been accomplished with the use of automated measurement of transepithelial electrical resistance in a study designed to assess the effects of e-cigarettes on the gut barrier and triggers of inflammation.7
Conclusion
Models that are based on 3D organoids and that better capture disease complexity have incredible potential in the identification and development of personalized therapies. Models that rely on engineered organ-in-a-dish systems allow for observation and manipulation of the complex relationships between the many components of human systems in a preclinical setting. A better understanding of the nuances that contribute to disease will guide the development of innovative medicines, with the hope of meeting—and exceeding— patient expectations in the clinical setting.
Soumita Das, PhD, is an associate professor of pathology and chief scientific director of the HUMANOID Center of Research Excellence and Pradipta Ghosh, MD, is a professor of medicine and cellular and molecular medicine, the executive director of the HUMANOID Center of Research Excellence, and the director of the Institute for Network Medicine at the University of California, San Diego. Elizabeth Abraham, PhD, is a senior product manager and Shabana Islam, PhD, is a product line manager at Corning Life Sciences.
References
1. Sherman H, Elliott N, White A, Rossi A. High Throughput Gene Expression Analysis of 3D Airway Organoids: Application Note. https://www.corning.com/catalog/cls/documents/application-notes/CLS-AN-534.pdf. Accessed March 23, 2021.
2. Slater K, Nandivada H. Culture of Mouse Intestinal Organoids in Corning® Matrigel® Matrix for Organoid Culture: Application Note. https://www.corning. com/catalog/cls/documents/application-notes/CLS-AN-542.pdf. Accessed March 23, 2021.
3. Sayed IM, Suarez K, Lim E, et al. Host engulfment pathway controls inflammation in inflammatory bowel disease. FEBS J. 2020; 287(18): 3967–3988. DOI: 10.1111/febs.15236.
4. Sayed IM, Sahan AZ, Venkova T, et al. Helicobacter pylori infection downregulates the DNA glycosylase NEIL2, resulting in increased genome damage and inflammation in gastric epithelial cells. J. Biol. Chem. 2020; 295(32): 11082–11098. DOI: 10.1074/jbc.RA119.009981.
5. Ghosh P, Swanson L, Sayed IM, et al. The stress polarity signaling (SPS) pathway serves as a marker and a target in the leaky gut barrier: implications in aging and cancer. Life Sci. Alliance 2020; 3(3): e201900481. DOI: 10.26508/ lsa.201900481.
6. Slater K, Flaherty P. Everything you ever wanted to ask about Corning® Matrigel® Matrix. Cell Culture Dish. October 2, 2017. https://cellculturedish.com/ everything-you-ever-wanted-to-ask-about-corning-matrigel-matrix/. Accessed March 9, 2021.
7. Sharma A, Lee J, Fonseca AG, et al. E-cigarettes compromise the gut barrier and trigger inflammation. iScience 2021; 24(2): 102035. DOI: 10.1016/j. isci.2021.102035.

