An international consortium of scientists that had been working on a way to determine the viability of batches of tiny liver organoids has devised a polygenic risk score (PRS) that shows when a drug—whether developmental or already approved—poses a risk of drug-induced liver injury (DILI). The researchers, including teams at Cincinnati Children’s Hospital Medical Center, Tokyo Medical and Dental University, Takeda Pharmaceutical in Japan, and research centers in Japan, Europe, and the United States, reported on their work in Nature Medicine.
The development of a PRS for DILI represents a major step towards solving a problem that has frustrated drug developers for years. “So far we have had no reliable way of determining in advance whether a medication that usually works well in most people might cause liver injury among a few,” said Jorge Bezerra, MD, who is director, division of gastroenterology, hepatology, and nutrition at Cincinnati Children’s, but who wasn’t involved in the study.
“That has caused a number of promising medications to fail during clinical trials, and in rare cases, also can cause serious injury from approved medications. If we could predict which individuals would be most at-risk, we could prescribe more medications with more confidence.” Takanori Takebe, MD, an organoid expert at Cincinnati Children’s, is corresponding author of the team’s published paper, which is titled, “Polygenic architecture informs potential vulnerability to drug-induced liver injury.”
Drug-induced liver injury is one of the primary reasons that drugs fail in development, or are withdrawn from the market, the authors wrote. “… this is partially due to the inability to identify patients who are at risk.” Genome-wide association studies (GWAS) carried out by the international Drug-Induced Liver Injury Consortium (iDILIC) and the Drug-Induced Liver Injury Network (DILIN) had previously identified gene variants that are associated with DILI linked with the use of different drugs. “Because each variant has modest predictive effect, we revisited GWAS findings to determine whether the PRS, which sums up the effects of numerous variants, informs potential DILI susceptibility in humans,” the authors explained. “The goal of this study was to develop PRSs using data from previous GWASs (performed by the iDILIC and the DILIN) and to validate their performance characteristics in GWAS data obtained from an independent clinical trial of a hepatotoxic drug, as well as multiple donor-derived organoids and primary hepatocytes treated with a variety of hepatotoxic medications.”
By combining the available data and applying several mathematical weighting methods, the team found a PRS formula that does appear to predict which patients may develop DILI as a result of taking different drugs. The final risk score takes into account more than 20,000 gene variants.
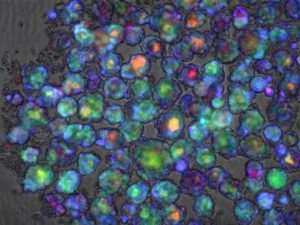
The researchers confirmed the score’s predictive power through studies in cell culture, in organoid tissue, and by using existing patient genomic data. They found that the PRS was valid in tests involving more than a dozen medications, including cyclosporine, bosentan, troglitazone, diclofenac, flutamide, ketoconazole, carbamazepine, amoxicillin-clavulanate, methapyrilene, tacrine, acetaminophen, and tolcapone. “This is the first unbiased analysis to implicate genetic variation at the level of the hepatocyte contributing to DILI susceptibility, validated in an independent clinical study, as well as unrelated donor-derived organoids and primary hepatocytes,” they stated. “The PRS predicted the susceptibility to DILI in patients treated with fasiglifam, amoxicillin–clavulanate, or flucloxacillin and in primary hepatocytes and stem cell-derived organoids from multiple donors treated with over ten different drugs.”
The PRS works for different types of drugs because it focuses on a set of common mechanisms involved in how the liver metabolizes a drug, including oxidant stress pathways in liver cells and endoplasmic reticulum (ER) stress—a disruption of cell function that happens when proteins cannot fold properly. “Pathway analysis highlighted processes previously implicated in DILI, including unfolded protein responses and oxidative stress,” the team commented.
The score could make it feasible for clinicians to run a genetic test, before prescribing medication, which would identify patients at higher risk of liver injury if they took the drug. The findings might result in the clinic making a change to drug dosage, order more frequent follow-up tests to catch early signs of liver damage, or switch medications entirely.
For drug research and development, the test could help to exclude from clinical trials those people at high risk of liver injury, so that the benefits of the drug being tested could be more accurately assessed. “Our genetic score will potentially benefit people directly as a consumer diagnostic-like application, such as 23andMe and others, suggested Takebe, who has been studying ways to grow liver “buds” for large-scale use in research. “People could take the genetic test and know their risk of developing DILI.” However, he acknowledged, more research involving a greater number of people will be needed to confirm the initial findings, and to scale up a DILI screening test for potentially widespread use.
Liver toxicity has caused a number of drug failures over the years. Takebe noted the withdrawal of a potential diabetes treatment, fasiglifam, in 2014, during Phase III clinical trials. Some of the participants (at a rate equivalent to about 1 in 10,000) experienced elevated enzyme levels that suggested potential liver injury. While such risks may appear low, at the time there was no way to predict which people would develop DILI, making the drug unacceptably dangerous. The new polygenic risk score would make it possible to produce liver organoids that exhibit key risk variants, to determine if a drug is harmful before people ever take it.
Takebe and colleagues demonstrated how to produce liver buds on a mass scale in 2017 in a study published in Cell Reports. The team subsequently improved upon the process, reporting in 2019 in Cell Metabolism, on their success at engineering liver organoids that model disease.



