Current treatments for hearing loss focus on amplifying sound, rather than targeting the cause of the disease. Now, a team of researchers report the use of base editors to treat Baringo mice—a mouse model of recessive genetic deafness caused by a point mutation in the transmembrane channel-like 1 gene Tmc1. This method, which is the first example of repairing a recessive gene mutation, restored hair cell sensory transduction and partial hearing.

Base editing is a technique developed by the lab of David Liu, PhD, director of the Merkin Institute of Transformative Technologies in Healthcare and professor of chemistry and chemical biology at Harvard University, that can specifically correct a common class of base substitutions without cleaving DNA. Base editing has the potential to provide restoration of gene function by directly repairing point mutations.
“This research is very important for the pediatric community here at Boston Children’s Hospital and elsewhere because about 4,000 babies are born each year with genetic hearing loss,” said Jeffrey Holt, PhD, director of otolaryngology research at Boston Children’s Hospital and co-senior author on the paper. “And, we feel this is a big step beyond the field of hearing restoration and for the broader field focused on the treatment of genetic disorders.”
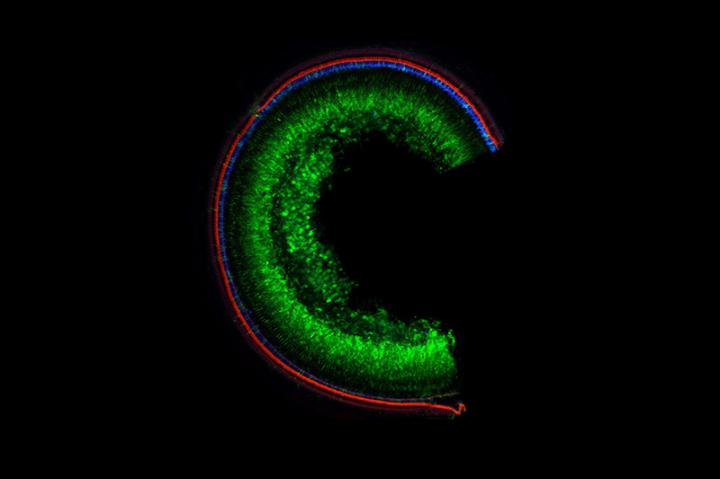
The gene editing method included a cytosine base editor inserted into a dual–adeno-associated virus (AAV) system, which was injected into the inner ear of the animals with hearing loss. The treatment reversed the mutation, improved sensory transduction, and partially restored hearing in mice, following a single injection of base editor AAVs. This technique opens the door to treating other genetic forms of hearing loss and other genetic diseases
Base editor acts as a spell-check
Earlier research in 2015 from the Holt lab and colleagues showed that replacing a full DNA sequence for Tmc1 into the sensory cells in the ear restores hearing in deaf mice. The Tmc1 protein is required for normal auditory function because it forms mechanosensitive ion channels in sensory hair cells of the inner ear.
“In that case, we used a single engineering AAV to deliver a functioning copy of the Tmc1 gene into the ear,” Holt said.
This research goes a step further. Instead of replacing a gene, the team repaired a single mutation in the Tmc1 gene converting it back to the correct sequence. “It’s like your spell-checker,” Holt explained. “If you type the wrong letter, spell checker fixes it for you.” When the team fixed the defect in the sensory cells in the ear, the edited cells recovered 100% of their function.
One limitation of AAV vectors is their limited capacity. In this case, the base editor was too large for a single AAV. As a result, the base editor sequence was split into two AAVs. The technique required the use of two viral vectors to deliver the base editing machinery. Cells with both vectors recovered 100% function.
“Once the cell was infected with these two parts, it was able to reassemble into a single full length sequence and then perform the base editing task we needed,” said co-first author Olga Shubina-Oleinik, PhD, a post-doctoral fellow at the Holt lab.
Although the approach worked when both AAVs made their way into the cell, that was the case in about one-quarter of the cells, which was enough to provide some hearing to the mice.
“We got it to work but we need to boost the efficiency to make it broadly useful,” said Holt. If only one AAV got into the cell, it did not work. “But the message is that when we got both into the cells, we went from zero function to 100%. That tells me all we need to do is get it into more cells and we will recover more hearing function.”
Building on previous success
At least 100 different genes are involved in hearing in the inner ear. Mutations in any one of those can lead to hearing loss.
“We have been developing different strategies targeting several of these different forms of hearing loss,” said Holt. “It really takes a precision medicine approach where we are trying to tailor our strategy specific, not just each gene that is involved, but in some cases the individual genetic mutation in the gene as is the case with this study.”
The Holt lab has a long history of success unraveling these genetic causes of hearing loss and developing gene therapy treatments for genetic forms of hearing loss. In 2011, the team first discovered that the Tmc1 protein is required for hearing and balance. After its 2015 success, the Holt team used CRISPR-Cas9 gene editing in 2019 to prevent hearing loss in Beethoven mice, a model of a dominant Tmc1 mutation.
Over 70 different mutations have been identified in the Tmc1 gene in humans. “We hope this new technique will allow us to pick them off one at a time to restore hearing and balance related to the inner ear,” said Holt.