Andrew Steckl, PhD, an Ohio eminent scholar and professor of electrical engineering in the University of Cincinnati’s (UC) college of engineering and applied science, working with researchers from Johns Hopkins University, said they have developed a new treatment for glioblastoma multiforme (GBM), an aggressive form of brain cancer. Steckl’s nanoelectronics laboratory applied an industrial fabrication process called coaxial electrospinning to form drug-containing membranes.
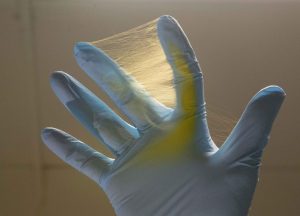
The treatment, which is implanted directly into the part of the brain where the tumor is surgically removed, can deliver a safe and effective dose of medicine for brain tumors without exposing patients to toxic side effects from traditional chemotherapy, according to the scientists, who published their study (“Multi-layered core-sheath fiber membranes for controlled drug release in the local treatment of brain tumor”) in Nature Scientific Reports.
“Interstitial chemotherapy plays a pivotal role in the treatment of GBM, an aggressive form of primary brain cancer, by enhancing drug biodistribution to the tumor and avoiding systemic toxicities. The use of new polymer structures that extend the release of cytotoxic agents may, therefore, increase survival and prevent recurrence. A novel core-sheath fiber loaded with the drug carmustine (BCNU) was evaluated in an in vivo brain tumor model. Three-dimensional discs were formed from coaxially electrospun fiber membranes and in vitro BCNU release kinetics were measured,” the investigators wrote.
“In vivo survival was assessed following implantation of discs made of compressed core-sheath fibers (NanoMesh) either concurrently with or five days after intracranial implantation of 9L gliosarcoma. Co-implantation of NanoMesh and 9L gliosarcoma resulted in statistically significant long-term survival (>150 days). Empty control NanoMesh confirmed the safety of these novel implants. Similarly, Day 5 studies showed significant median, overall, and long-term survival rates, suggesting optimal control of tumor growth, confirmed with histological and immunohistochemical analyses. Local chemotherapy by means of biodegradable NanoMesh implants is a new treatment paradigm for the treatment for brain tumors. Drug delivery with coaxial core-sheath structures benefits from high drug loading, controlled long-term release kinetics, and slow polymer degradation. This represents a promising evolution for the current treatment of GBM.”
“Chemotherapy essentially is whole-body treatment. The treatment has to get through the blood-brain barrier, which means the whole-body dose you get must be much higher,” Steckl said. “This can be dangerous and have toxic side-effects. By selecting the base materials of the fiber and the thickness of the sheath, we can control the rate at which these drugs are released.”
The electrospun fibers can rapidly release one drug for short-term treatment such as pain relief or antibiotics while an additional drug or drugs such as chemotherapy is released over a longer period, he said, adding that “we can produce a very sophisticated drug-release profile.”
The breakthrough is a continuation of work conducted by research partners and co-authors Henry Brem, MD, and Betty Tyler, MD, at Johns Hopkins, who in 2003 developed a locally administered wafer treatment for brain tumors called Gliadel, noted Steckl.
Unlike previous treatments, electrospun fibers provide a more uniform dose over time, explained UC research associate Daewoo Han, PhD, the study’s lead author. “For the current treatment, most drugs release within a week, but our discs presented the release for up to 150 days,” Han said.
The electrospun fiber created for the study provided a tablet-like disk that increased the amount of medicine that could be applied, lowered the initial burst release and enhanced the sustainability of the drug release over time, the study found. Chemotherapy using electrospun fiber improved survival rates in three separate animal trials that examined safety, toxicity, membrane degradation, and efficacy, the researchers said.
While this study used a single drug, the team noted that one advantage of electrospinning is the ability to dispense multiple drugs sequentially over a long-term release. The latest cancer treatments rely on a multiple-drug approach to prevent drug resistance and improve efficacy.
Steckl said the study holds promise for treatments of other types of cancer.
“Looking ahead, we are planning to investigate ‘cocktail’ therapy where multiple drugs for the combined treatment of difficult cancers are incorporated and released either simultaneously or sequentially from our fiber membranes,” Steckl said.


