Seemingly ordinary bacteria may act like sleeper agents, appearing relatively innocuous during clinical tests while retaining their potential for antibiotic resistance. If activated after passing the tests, sleeper agent bacteria may reassert their capacity for antibiotic resistance with a vengeance.
This nefarious bit of microbial tradecraft has been dubbed Silencing of Antibiotic Resistance by Mutation (SARM) by scientists based at the University of Leeds. The scientists, led by Alex J. O’Neill, PhD, associate professor, identified SARM as a challenge after following up on sporadic reports of bacteria harboring antibiotic resistance genes that become inactivated (temporarily) as a result of a genetic mutation.
“Our findings highlight the fact that antibiotic resistance can sometimes effectively be hidden,” said O’Neill. “In other words, it looks like you’re dealing with an infection that should be treatable with a given antibiotic, but that may not be the case.”
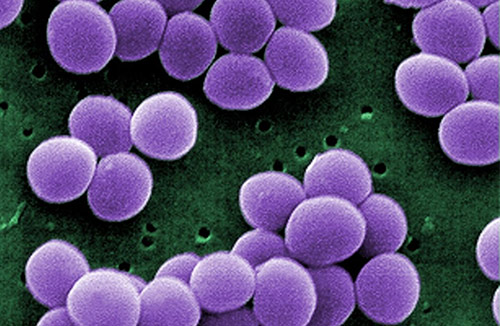
O’Neill and colleagues described how they isolated SARM strains in a paper (“Transient Silencing of Antibiotic Resistance by Mutation Represents a Significant Potential Source of Unanticipated Therapeutic Failure”) that appeared October 29 in the journal mBio. According to the paper, the researchers analyzed nearly 1470 samples of Staphylococcus aureus—a bacteria that is commonly found on the skin but can cause more serious infections and toxic-shock syndrome. It is best known in its highly drug-resistant form, MRSA, which frequently causes a potentially lethal hospital-acquired infection.
“Of the isolates analyzed, 152 (10.3%) harbored a silenced resistance gene, including 46 (3.1%) that exhibited SARM to currently deployed antistaphylococcal drugs,” the article’s authors wrote. “SARM resulted from diverse mutational events but most commonly through frameshift mutation of resistance determinants as a result of point deletion in poly(A) tracts.”
O’Neill and colleagues also found that in 9 out of 10 samples where SARM was identified, the effect of the mutation was quickly lost when the bacteria were exposed to antibiotics. This was due to a process called “reversion”—in effect a second mutation which restored the pathogen to its original, drug-resistant state. Although the study only looked at S. aureus, the researchers believe it is likely that this process also occurs on other bacteria.
“The ease with which SARM strains become drug-resistant means that they are ‘wolves in sheep’s clothing,’” O’Neill emphasized. “SARM is therefore a potentially important reason why antibiotic treatments fail unexpectedly in infected patients.
“We hope that our study will alert doctors to the knowledge that silenced antibiotic resistance genes are relatively common in bacteria such as S. aureus, and therefore have significant potential to adversely affect antibiotic treatment.”
The research reveals a weakness in the routine screening process for drug-resistant bacteria. Bacteria isolated from patients with a serious infection undergo what is known as susceptibility testing—tests to determine which antibacterial drugs will be effective in attacking the infection. This is the gold-standard approach, but the research reveals how the test is “blindsided” in SARM strains where the resistance gene is dormant.
“SARM can be detected using DNA sequencing to determine the complete genetic make-up of strains,” O’Neill pointed out, “but this technology is not yet in routine use in clinical microbiology laboratories.”
In their concluding remarks, O’Neill and colleagues argued that until DNA sequencing is in common use to detect SARM, this “hidden” form antibiotic resistance should be investigated, whenever practicable, as a potential cause in cases of unanticipated therapeutic failure in the treatment of bacterial infection.