A pilot study in obese and overweight human volunteers has found that a dietary supplement comprising a pasteurized gut bacterium can help to improve key metabolic parameters that may reduce the risk of diabetes and cardiovascular disease. The study, carried out by researchers at the Louvain Drug Research Institute of the University of Louvain, and the Cliniques Universitaires Saint-Luc, showed that oral supplements of the pasteurized Akkermansia muciniphila bacterium limited the increase of several risk factors for cardiovascular disease, moderated the progression of pre-diabetes, and reduced cholesterol levels in humans. The researchers are now planning larger-scale studies and aim to market pasteurized Akkermansia muciniphila as a food supplement, possibly within the next couple of years.
Clara Depommier, PhD, is lead author of the team’s paper describing the human study, which is published in Nature Medicine, and titled, “Supplementation with Akkermansia Muciniphila in overweight and obese human volunteers: a proof-of-concept exploratory study.” The authors concluded, “This study provides a promising start for the development of future clinical interventions with appropriate design to confirm and extend our findings, which show the safety and impact of oral supplementation with A. muciniphilain overweight or obese insulin-resistant individuals.”
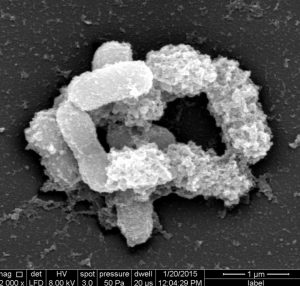
The intestinal bacterium A. muciniphila has attracted considerable interest for its potential health-promoting effects. Back in 2007, a UCLouvain team headed by senior study author Patrice Cani, PhD, a FNRS-WELBIO researcher and working with co-corresponding author Willem de Vos, PhD, a professor at the University of Wageningen, demonstrated that A. muciniphila could moderate the development of obesity and type 2 diabetes in mice. Ten years later the team “serendipitously” discovered that giving mice a pasteurized form of Akkermansia, rather than the live bacterium, resulted in even greater protection against key cardiovascular disease risk factors such as insulin resistance, hypercholesterolemia, and adiposity.
However, it wasn’t known whether supplements of the pasteurized bacterium would have similar benefits in humans. To be able to test this in a small-scale study, the team first had to develop a process using a synthetic growth medium that would be suitable for manufacturing the bacterium for human administration. They then designed a proof-of-concept study to investigate the feasibility, safety, and tolerance of A. muciniphila supplements, and also to evaluate for the first time the metabolic effects of A. muciniphila supplements in humans.
The randomized, double-blind, placebo-controlled pilot study included 40 overweight or obese volunteers with insulin resistance, 32 of whom completed the trial. The volunteers were randomized into three groups, which were given daily oral supplements of either placebo, live A. muciniphila, or pasteurized A. municiphila, for three months. The participants were asked to keep to their regular diets and not to change their normal levels of physical activity. “The primary endpoints were safety, tolerability, and metabolic parameters (that is, insulin resistance, circulating lipids, visceral adiposity, and body mass),” the investigators explained. “Secondary outcomes were gut barrier function (that is, plasma lipopolysaccharides) and gut microbiota composition.”
Recent studies have found that oral A. muciniphila administration can reduce plasma cholesterol in rodents and can also prevent the development of atherosclerosis in the animal model. Encouragingly, results from the new human study showed that “administration of pasteurized A. muciniphila significantly decreased total cholesterol by 8.68% compared to placebo, whereas low-density lipoprotein (LDL) cholesterol was 7.53% lower and triglycerides were 15.71% lower, but did not reach significance.”
In contrast to the positive effects of A. muciniphila supplements on multiple metabolic parameters, a deterioration in insulin resistance and hypercholesterolemia was seen in the participants who were randomized to take placebo. Importantly, A. muciniphila supplementation didn’t lead to any observed changes in global changes to gut microbiota. “… these results demonstrate that supplementation with either pasteurized or live A. muciniphila did not affect the overall structure of the gut microbiome,” they wrote. “This finding is in line with previous data obtained in rodents, which showed that the gut microbiome of mice supplemented with live A. muciniphila was not significantly modified.
The team acknowledged that the reported clinical study did have some limitations, including its small size, which meant that it wasn’t powered to allow definitive conclusions on endpoints relating to metabolic parameters. “Although most of the primary outcomes were reached, we did not find significant changes in visceral adiposity and BMI,” the scientists also noted. Nevertheless, they concluded, “this proof-of-concept prospective study shows the feasibility of culturing and administering A. muciniphila to humans. Our data unequivocally show that administration of a daily dose as high as of 1010 cells of A. muciniphila is safe in the longer term (that is, three months) … and that supplementation with A. muciniphila improves several metabolic parameters.”



