Scientists in Canada have used CRISPR-Cas9 technology to identify potential new targets for glioblastoma (GBM), the most common type of primary brain tumor in adults. The approach used genome editing to effectively reverse engineer patient-derived, tumor-propagating glioblastoma stem cells (GSCs) gene by gene, and identify genes that are essential for tumor growth. In addition to highlighting a number of possible glioblastoma targets, the studies provided new insights into the basis of glioblastoma resistance to temozolomide (TMZ) chemotherapy, and potential strategies for combination treatment.
“This is one of the first studies of its kind, where CRISPR screens are performed directly in multiple freshly isolated patient cells in parallel,” commented research co-lead Stéphane Angers, PhD, a professor at the Leslie Dan Faculty of Pharmacy, University of Toronto. “This study has provided a massive amount of new information that the research community can now interrogate to help design new treatment strategies.” Angers, together with lead author Graham MacLeod, a post-doctoral fellow at University of Toronto’s Leslie Dan Faculty of Pharmacy, and colleagues at the University of Toronto, the Hospital of Sick Children, and the University of Calgary, reported their findings in an open access paper in Cell Reports, which is titled, “Genome-Wide CRISPR-Cas9 Screens Expose Genetic Vulnerabilities and Mechanisms of Temozolomide Sensitivity in Glioblastoma Stem Cells.”
Glioblastoma demonstrates significant heterogeneity between patients, but also in the same patient, the authors explained. This variation, combined with “a complete lack of durable responses to therapy” means that GBM has a “dismal overall prognosis.” Even temozolomide, which represents the latest form of chemotherapy for this tumor type, demonstrates what the researchers term “remarkably limited” efficacy. “These glioblastoma stem cells are also resistant to treatment, which is one reason that these tumors are so hard to cure,” noted Peter Dirks, PhD, research co-lead and staff neurosurgeon and senior scientist at the Hospital for Sick Children. “We need new ways to disrupt these cells specifically if we are going to give people a better chance of survival.” There are in addition concerns that TMZ can cause cancer cells to develop new mutations that may actually drive disease progression.
“Indeed, a more comprehensive understanding of molecular determinants of growth and drug responsiveness across this heterogenous cancer is needed, both to identify new potential treatments and to provide new strategies that could be partnered with TMZ, which is now entrenched in upfront GBM therapy,” the team stated.
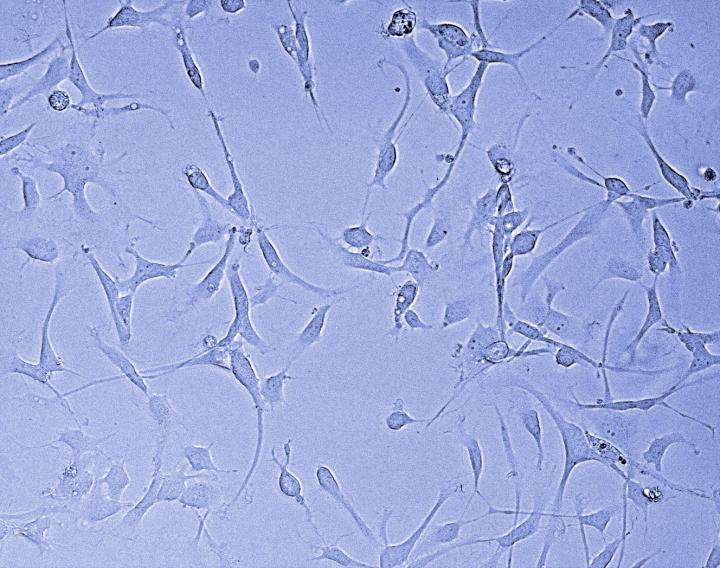
Scientists believe that GBM growth is driven by a small population of stem cells within the tumors, and culture systems for patient-derived GSCs have allowed scientists to investigate the basis and progression of GBM in greater depth. “Importantly, these GSC cultures reliably preserve patient-specific phenotypic and genotypic characteristics,” including their in vivo tumorigenic capacity and growth behaviors,” the researchers commented. CRISPR gene editing tools can also be used to carry out “cell fitness screens” that identify both “core” and “context-specific” essential/fitness genes that control cell proliferation.
Given the heterogeneity of GBM between patients, the University of Toronto-led team carried out parallel genome-wide CRISPR screens in 10 unique patient-derived GSC cultures, to try and identify the molecular basis of cell growth and survival. The approach basically involved systematically knocking down each of the 20000 genes, one at a time, from each patient sample, to see the effect on tumor growth and survival. They compared data from the GSC screens with those from parallel screens on two normal human fetal neural stem cell cultures. Separate chemogenomic screens were carried out to identify these genes involved in tumor resistance to TMZ and potential strategies for combination therapies.
“Cancer stem cells fuel the growth of tumors and progression of the disease,” said Angers. “In order to effectively target these cells, having a comprehensive view of the genes controlling the growth programs is critical. If you know which genes are necessary for these cells to survive and proliferate, you can then look at ways to attack or block these genes and stop tumor growth in its tracks.”
The results highlighted members of the SOX transcription factor family, SOCS3, USP8 and DOT1L, and protein ufmylation pathway genes as important for GSC growth and fitness. “The identification of common GSC fitness genes, despite inherent intratumoral heterogeneity and irrespective of patient tumor genotype, provides insight into the underlying biology of GBM and identifies potential avenues for preclinical evaluation,” the authors wrote.

The screens also identified multiple stress signaling pathways as essential for the growth of GSCs, something that the team acknowledged was a particularly “exciting finding.” “Together with previous studies, this supports further investigation of the effectiveness of therapeutic strategies targeting JNK signaling for GBM,” they wrote. “Despite interpatient heterogeneity in GBM, the finding of common essential programs for GSC growth and survival lends hope that we will develop therapies that can be used on larger groups of GBM patients, with patient-specific vulnerabilities providing complementary personalized strategies.”
The team separately carried out additional CRISPR-Cas9 screens in patient-derived GBM cultures to identify genes involved in intrinsic resistance to TMZ. Their findings highlighted genes involved in the Fanconi anemia pathway, a biochemical network that is involved in processes including DNA repair and DNA replication, and also identified genes involved in base excision repair and nucleotide excision repair, although not all the genes were conserved across all the GSC cultures.
“In summary, our genome-wide CRISPR screens in patient-derived GSC cultures have identified a diversity of genetic vulnerabilities and contain a wealth of data that can be further mined to identify drug targets for GBM,” the authors concluded. “Future studies will seek to identify the precise mechanism by which these genes and pathways modulate the fitness and/or chemosensitivity of GSCs, and whether they contribute to disease progression in vivo.”