A liquid biopsy is a simple noninvasive alternative to tissue biopsies in which a body fluid specimen is obtained for detailed laboratory analyses. Tissue biopsy has been used to characterize diseased tissue or for diagnosis. Although it is the most direct method, it is limited by constraints on sampling frequency and because it is an incomplete representation of the entirety of the organ. A liquid biopsy for cancer detection or management is an old concept with a new twist. Tumor cells were first found in circulation in the late 19th century, and the term “cell-free DNA (cfDNA),” which referred to fragmented DNA found outside cells in the blood, was first reported by Mandel and Metais in 1948 (Mandel and Metais, 1948). Then, work in the 1970s revealed that patients with cancer tended to have an increased concentration of cfDNA in their blood (Leon et al., 1977). The advent of powerful high-sensitivity DNA detection and analysis tools, and an increased understanding of molecular oncology—such as the comprehensive molecular profiles from hundreds of tumors in The Cancer Genome Atlas, and the generation of targeted therapeutic agents have fueled insights to potential clinical applications for cfDNA to cancer treatment. This “genomics-driven or precision oncology” using liquid biopsies has been summarized in recent reviews by Corcoran and Chabner (2018), Heitzer et al. (2018), and others. Liquid biopsies have become a highly topical field, with rapid advances toward improving the diagnoses and prognoses of not only oncology but also nearly every type of disease and from nearly every organ system.
Although tumor-related liquid biopsy has most often referred to the analysis of cfDNA from peripheral blood, it also encompasses other tumor-derived materials (e.g., circulating tumor RNA, proteins and some metabolites, circulating extracellular vesicles such as exosomes, or intact circulating tumor cells from blood and other bodily fluids). Together, these analytes have the potential to provide information about the existence and/or features of tumors in various stages and can be used to generate “omics information” including genomes, epigenomes, transcriptomes, proteomes, and metabolomes. Liquid biopsies, particularly those involving cfDNA from plasma, are rapidly emerging as an important and minimally invasive adjunct to standard tumor biopsies and, in some cases, as an alternative approach. To date, liquid biopsies have been used for colorectal cancer, breast cancer, and lung cancer to predict patient responses to therapy and to monitor relapses for clinical care.
One obstacle to cancer management is the way that cancer can evolve. Tumor genetic diversity and evolution constantly happen. This allows cancers to adapt to changing environments, survive treatments, and spread. To improve treatment, physicians must track the cancer’s genetic shifts in real time and analyze tumors during therapy. In theory, it should then be possible to tailor a regimen to emerging patterns of resistance and relapse if such treatments are available. The potential of liquid biopsies is highlighted by studies that show that they can track the evolutionary dynamics and heterogeneity of tumors and can detect very early emergence of therapy resistance, residual disease, and recurrence (Abbosh et al., 2017; Jamal-Hanjani et al., 2017). Therefore, in theory, liquid biopsy provides a way to track tumor evolution in a noninvasive and more comprehensive way that is beyond the reach of existing tissue biopsies. The advantages, in principle, of liquid over standard surgical biopsies are indisputable. They are noninvasive, simple to administer, more patient-friendly, overcome the problem of heterogeneity in tumor makeup, and, by serial testing, allow the progression of a tumor to be more easily followed to help inform treatment decisions. Of course, before these goals can be achieved, liquid biopsies must pass rigorous analytic validation to reach high clinical utility.
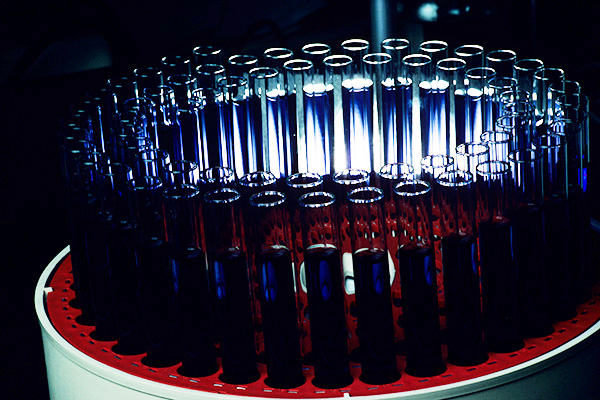
One of the challenges is to determine whether the mutational profile established through cfDNA testing reliably reproduces the mutational profile derived from a direct tumor biopsy, the current standard of care. It is thought that cfDNA is released into the blood stream through apoptosis or necrosis and found as double-stranded fragments of ∼150–250 bp in length, corresponding to nucleosome-associated DNA (Fan et al., 2010). Interestingly, this circulation-derived nucleosome-sized 150–250 bp cfDNA was also reported in urine about a decade ago (Su et al., 2004), as reviewed by Jain et al. in this issue. In patients with cancer, cfDNA from tumor cells (circulating tumor DNA [ctDNA]) constitutes only a fraction of the overall cfDNA, and this fraction varies greatly between individuals from <0.1% to >90%, possibly due to differences in tumor burden and the rate of cell death in individual tumors (Diehl et al., 2008; Bettegowda et al., 2014). Due to the low levels and short half-life of ctDNA, specialized approaches are needed for sample collection, storage, isolation, and analysis of ctDNA. Thus, detection and analysis of ctDNA present a considerable challenge, as highlighted in recent studies, discussed below.
Early studies found low concordance between alterations detected in tumor and plasma samples from the same patients and even between results from the same blood samples tested with different commercial assays (Chae et al., 2016; Kuderer et al., 2017; Torga and Pienta, 2017). However, nonconcordance was most often observed in patients with low ctDNA levels. Encouragingly, larger and more carefully controlled studies showed high concordance rates of 80–90% between plasma and tissue samples in key cancer driver genes (Adalsteinsson et al., 2017; Schrock et al., 2018). Of note, the dynamics of ctDNA levels may themselves be of pathological significance and should be considered a biomarker along with other biomarkers and tumor-related genetic alterations in a liquid biopsy. In tissue biopsies, adjacent nontumor tissue often serves as “internal non-tumor control,” but an internal control in liquid biopsies has yet to be established.
Of public interest, a study by Cohen et al. (2018) used a test called CancerSEEK that showed promise for cancer screening by liquid biopsies. In their cohort of more than 1000 patients with cancer and about 800 healthy controls, they achieved an overall median sensitivity to cancer of 70%. One challenge for liquid biopsies for cancer screening is determining the tumor site in the body. Cohen et al. suggested that individuals who test positive twice by liquid biopsy should undergo imaging to find the tumor site. The identification of the organ site may also be narrowed by using tailored markers such as alpha-fetoprotein for liver cancer or based on patient history, such as if the patient is hepatitis B virus infection-positive and therefore at risk for liver cancer. Once targeted therapies with low toxicity are available, the administration of targeted therapy to those with positive test results may be possible without knowing the tumor site.
The advent of “omics” for various analytes generates a large amount of data that must be processed with sophisticated statistical modeling methods for meaningful analysis. Machine learning methods offer opportunities to build cancer detection classifiers (Kourou et al., 2015; Wang et al., 2018) that can be continually improved as more data become available.
While promising, many challenges remain in the use of liquid biopsies from sample collection to data analysis. It is critical that biomarkers are kept viable during the sample preparation and DNA isolation process. When detecting biomarkers, researchers must be cognizant that undetected biomarkers only suggest either that the level of the biomarker is below the limit of detection of a given assay or that the biomarker was lost upstream of the analysis during sample collection, storage, or DNA isolation. As a result, positive data are currently more meaningful than negative data in liquid biopsies. Repeated sampling is one approach that can be taken to mitigate this challenge.
Liquid biopsy has increasingly been adopted and explored for clinical care, but careful analytic and clinical validation, as well as additional preclinical studies addressing the biology of liquid biopsy analytes, still need to be performed. While most existing assays have focused on a single analyte or specific DNA alterations, resolution and robustness may be improved by adopting multiple analytes, by examining DNA alterations more generally, by repeat sampling from the same individual to establish a healthy baseline, or even by including more than one type of body fluid. Platform technology for analyte analysis must be incorporated with novel and powerful tools, such as use of machine learning approaches to integrate the large amounts of data obtained. Thus, future liquid biopsy development is expected to involve basic biology, an improved understanding of biomarkers, assay development, statistics, computational machine learning, and sophisticated multicenter clinical validation studies. Last, but not least, these tests need to follow regulatory guidelines to establish assay performance and analytic validity. It is only after analytic validity and clinical utility have been established that liquid biopsies can be expected to impact cancer screening and precision oncology.
For references please access the original article An Old Concept with a New Twist.
Genetic Testing and Molecular Biomarkers, published by Mary Ann Liebert, Inc., is the leading peer-reviewed journal covering all aspects of human genetic testing including molecular biomarkers. The above article was first published in the April 2019 Liquid Biopsy special issue of Genetic Testing and Molecular Biomarkers. The views expressed here are those of the authors and are not necessarily those of Tissue Engineering, Mary Ann Liebert, Inc., publishers, or their affiliates. No endorsement of any entity or technology is implied.