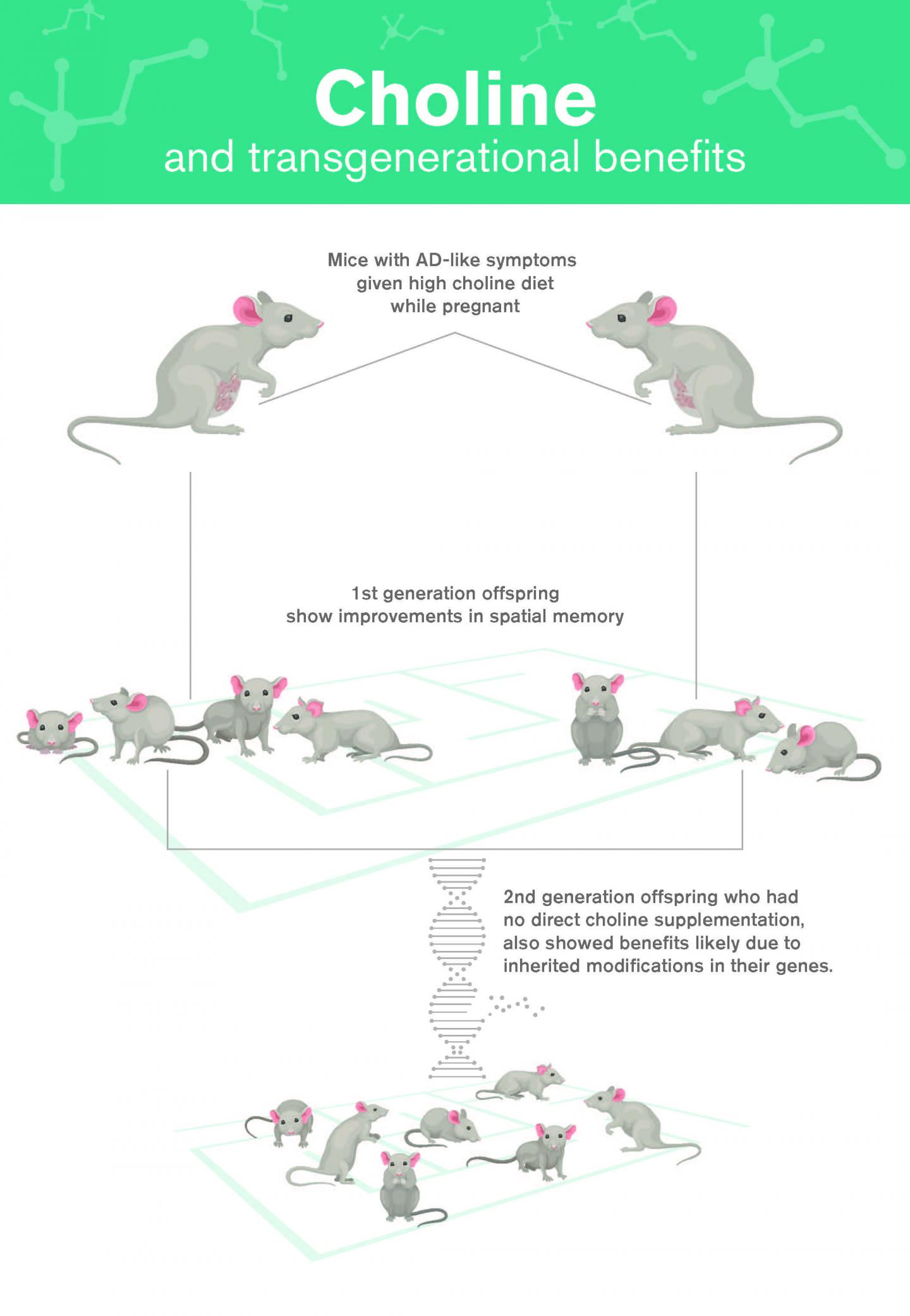
Could simple adjustments to dietary intake have a dramatic effect on preventing Alzheimer’s disease (AD) across generations? New evidence in mice from Biodesign Institute investigators at Arizona State University (ASU) would suggest that it’s possible. The ASU researchers found that mice bred to display AD-like symptoms, who were given high choline in their diet, bred offspring that showed marked improvements in spatial memory, compared with mice receiving a normal choline regimen in the womb. Findings from the new study were published today in Molecular Psychiatry through an article titled “Maternal choline supplementation ameliorates Alzheimer’s disease pathology by reducing brain homocysteine levels across multiple generations.”
Amazingly, the researchers found that the beneficial effects of choline supplementation appear to be transgenerational, not only protecting mice receiving choline supplementation during gestation and lactation, but also the subsequent offspring of these mice. While this second generation received no direct choline supplementation, they nevertheless reaped the benefits of treatment. The exploration of such epigenetic alterations may further excite new avenues of research and suggest ways of treating a broad range of transgenerational afflictions, including fetal alcohol syndrome and obesity.
Choline acts to protect the brain from AD in at least two ways, both of which are explored in the new study. First, choline reduces levels of homocysteine, an amino acid that can act as a potent neurotoxin, contributing to the hallmarks of AD: neurodegeneration and the formation of amyloid plaques.
Secondly, choline supplementation reduces the activation of microglia—cells responsible for clearing away debris in the brain. While their housekeeping functions are essential to brain health, activated microglia can get out of control, as they typically do during AD. Over-activation of microglia causes brain inflammation and can eventually lead to neuronal death. Choline supplementation reduces the activation of microglia, offering further protection from the ravages of AD.
AD is poised to afflict 13.5 million people in the U.S. alone by mid-century if nothing is done to address the disease. The staggering costs of Alzheimer’s are projected to exceed $20 trillion in the next 40 years. So, developing effective treatments rooted in a more thorough understanding of this complex disease is one of the most daunting challenges facing modern medicine and the global healthcare infrastructure.
Research into the origins of Alzheimer’s disease strongly suggests that a great variety of factors are at play. While advancing age remains the greatest risk factor, other hazards that have been implicated in the disease include genetic predisposition and lifestyle. Many studies have suggested that diet can have a significant effect in increasing or lowering the risk of cognitive decline, and the risks may be transmitted across generations.
Recent data has shown that a healthy diet has been shown to offer protection from diseases, including cancer and Alzheimer’s disease. For instance, patients following a Mediterranean diet for 4.5 years lowered their risk of AD by 54%. Another study pointed to the effects of a Mediterranean diet rich in fruits and vegetables, whole grains, legumes, and nuts, as well as fish and poultry in reducing the accumulation of Aβ-amyloid, the protein responsible for plaque formation.
Choline is a vitamin-like essential nutrient that is naturally present in some foods and available as a dietary supplement. It is a source of methyl groups needed for many steps in metabolism. All plant and animal cells require choline to maintain their structural integrity, Moreover, choline is used by the body to produce acetylcholine, an important neurotransmitter essential for brain and nervous system functions including memory, muscle control, and mood. It has long been recognized that choline is particularly important in early brain development. Pregnant women are advised to maintain choline levels of 550 mg per day for the health of their developing fetus.
“There’s a twofold problem with this,” explains lead study investigator Ramon Velazquez, PhD, a neuroscientist at ASU Biodesign Institute. “Studies have shown that about 90% of women don’t even meet that requirement. Choline deficits are associated with failure in developing fetuses to fully meet expected milestones like walking and babbling. But we show that even if you have the recommended amount, supplementing with more in a mouse model gives even greater benefit.”
Indeed, when the AD study mice received supplemental choline in their diet, their offspring showed significant improvements in spatial memory, which was tested in a water maze. Subsequent examination of mouse tissue extracted from the hippocampus, a brain region known to play a central role in memory formation, confirmed the epigenetic alterations induced by choline supplementation. Modified genes associated with microglial activation and brain inflammation and reduced levels of homocysteine resulted in the observed performance improvements in spatial memory tasks.
Remarkably, due to the epigenetic modifications induced by choline, the improvements carried over to the offspring of mice receiving supplemental choline in the womb.
“We found that early choline supplementation decreased homocysteine while increasing methionine, suggesting that high choline levels convert homocysteine to methionine,” Velazquez states. “This conversion happens thanks to an enzyme known as betaine-homocysteine methyltransferase (BMHT). We found that choline supplementation increased the production of BMHT in two generations of mice”
While much more work needs to be done to see if these results are transferrable to humans, the study’s significance is twofold, establishing beneficial effects from nutrient supplementation in successive generations and proposing epigenetic mechanisms to account for the reduction of AD memory deficit in mice.
“No one has ever shown transgenerational benefits of choline supplementation,” Velazquez concludes. “That’s what is novel about our work.”



