
Carbon monoxide (CO) is best known as a potentially deadly gas, but it also has immunomodulatory effects, and in small doses can reduce inflammation and help to stimulate tissue regeneration. A team of researchers led by MIT, Brigham and Women’s Hospital, the University of Iowa, and Beth Israel Deaconess Medical Center, has now devised a novel way to deliver carbon monoxide to the body that bypasses potentially hazardous effects. Inspired by techniques used in molecular gastronomy, the researchers incorporated CO into stable foams, or gas-entrapping materials (GEMs) that can be delivered to the digestive tract.
The researchers’ studies showed that these materials can trap and deliver CO to the intestines in different animal models, alleviating gut injuries such as colitis and radiation-induced gut damage. These new materials could address the lack of safe delivery routes for CO and facilitate clinical use of the gas across an array of conditions.
“The ability to deliver a gas opens up whole new opportunities of how we think of therapeutics,” said Giovanni Traverso, MD, PhD, who is the Karl van Tassel career development assistant professor of mechanical engineering at MIT, and a gastroenterologist at Brigham and Women’s Hospital. “We generally don’t think of a gas as a therapeutic that you would take orally (or that could be administered rectally), so this offers an exciting new way to think about how we can help patients.”
Traverso, and Leo Otterbein, PhD, a professor of surgery at Harvard Medical School and Beth Israel Deaconess Medical Center, are senior authors of the team’s published paper in Science Translational Medicine, which is titled, “Delivery of therapeutic carbon nonoxide by gas-entrapping materials.” The lead authors are James Byrne, MD, PhD, a physician-scientist and radiation oncologist at the University of Iowa (formerly a resident in the Mass General Brigham/Dana Farber Radiation Oncology Program), and a research affiliate at MIT’s Koch Institute for Integrative Cancer Research; David Gallo, a researcher at Beth Israel Deaconess; and Hannah Boyce, a research engineer at Brigham and Women’s.
CO is an odorless and colorless gas that has long been recognized as “a silent killer,” the authors wrote. When inhaled at high concentrations, carbon monoxide binds to hemoglobin (Hb) in the blood, displacing oxygen and forming carboxyhemoglobin (COHb), which decreases the body’s oxygen carrying capacity, potentially leading to serious health effects and even death. “In general, if COHb reaches 50%, then it may result in coma, convulsions, depressed respiration, and cardiovascular status or even fatal consequences,” the investigators continued.
In contrast, at lower doses, CO can have beneficial effects, such as reducing inflammation and promoting tissue regeneration. Since the late 1990s, Otterbein has been studying the therapeutic effects of low doses of carbon monoxide. The gas has been shown to impart beneficial effects in preventing rejection of transplanted organs, reducing tumor growth, and modulating inflammation and acute tissue injury. “Exogenous administration of CO has been beneficial for the treatment of many diseases in preclinical models, including cardiovascular disorders, sepsis and shock, acute lung, kidney, and liver injury, infection, and cancer,” the authors continued.
“We’ve known for years that carbon monoxide can impart beneficial effects in all sorts of disease pathologies, when given as an inhaled gas,” Otterbein added. “However, it’s been a challenge to use it in the clinic, for a number of reasons related to safe and reproducible administration, and health care workers’ concerns, which has led to people wanting to find other ways to administer it.” As the authors explained, “Inhalational delivery, however, presents profound challenges because of the variability in patient ventilation, environmental safety concerns for patients and healthcare workers, and the need for large amounts of compressed CO gas in cylinders that pose a health hazard due to the potential for cylinder leak or rapid depressurization.
A few years ago, Traverso and Otterbein were introduced by Christoph Steiger, PhD, a former MIT postdoc and a co-author of the newly reported study. Traverso’s lab specializes in developing novel methods for delivering drugs to the gastrointestinal tract. To tackle the challenge of delivering a gas, they came up with the idea of incorporating the gas into a foam, much the way that chefs use carbon dioxide to create foams infused with fruits, vegetables, or other flavors.
“The discipline of molecular gastronomy has inspired delectable gas-filled materials over the past 40 years,” the scientists noted. “Chefs across the world … have used foams and meringues to capture unique tastes and textures that appeal to the senses.” However, the authors continued, “The techniques from molecular gastronomy have seldom been translated for pharmacologic intent and provide a unique opportunity to enable delivery of CO and other gasotransmitters across the epithelium of the GI tract.”
Culinary foams are usually created by adding a thickening or gelling agent to a liquid or a solid that has been pureed, and then either whipping it to incorporate air or using a specialized siphon that injects gases such as carbon dioxide or compressed air.
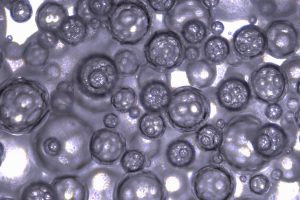
The MIT team created a modified siphon that could be attached to any kind of gas cannister, allowing them to incorporate carbon monoxide into their foam. To create the foams, they used food additives such as alginate, methyl cellulose, and maltodextrin. Xantham gum was also added to stabilize the foams. By varying the amount of xantham gum, the researchers could control how long it would take for the gas to be released once the foams were administered.
After showing that they could control the timing of the gas release in the body, the researchers tested the foams for different applications. First, they studied two types of topical applications, analogous to applying a cream to soothe itchy or inflamed areas. In a study of mice, they found that delivering the foam rectally reduced inflammation caused by colitis or radiation-induced proctitis (inflammation of the rectum that can be caused by radiation treatment for cervical or prostate cancer).
Current treatments for colitis and other inflammatory conditions such as Crohn’s disease usually involve drugs that suppress the immune system, which can make patients more susceptible to infections. Treating those conditions using a foam that can be applied directly to inflamed tissue offers a potential alternative, or complementary approach, to those immunosuppressive treatments, the researchers suggested. For their reported study, the foams were administered rectally, but it could also be possible to deliver them orally. “The foams are so easy to use, which will help with the translation to patient care,” said Byrne.
The researchers then set out to investigate possible systemic applications, in which carbon monoxide could be delivered to remote organs, such as the liver, because of its ability to diffuse from the GI tract elsewhere in the body. “We tested our formulations in three small animal models associated with inflammation and oxidative stress–induced tissue injury: acetaminophen (APAP)–induced acute liver injury, experimental colitis, and radiation-induced proctitis,” they wrote.
For one part of the study, the team used a mouse model of acetaminophen overdose, which causes severe liver damage. They found that gas delivered to the lower GI tract was able to reach the liver and greatly reduce the amount of inflammation and tissue damage. “Animals that received foam GEM were found to have a dose-dependent reduction in hepatocellular injury as measured by serum alanine aminotransferase (ALT) concentration compared to controls that received air GEM or no treatment,” the scientists stated.
The results of another set of experiments in mice with induced colitis supported the therapeutic benefits of the CO GEM formulation in limiting tissue damage in the colon. In a separate rat model of radiation-induced proctitis, rectal administration of the foam GEMs before and after radiation resulted in reduced intestinal crypt injury.
The researchers did not find any adverse effects after the carbon monoxide administration in their reported experiments. Previous studies in humans have shown that small amounts of carbon monoxide can be safely inhaled. A healthy individual has a carbon monoxide concentration of about 1% in the bloodstream, and studies of human volunteers have shown that levels as high as 14% can be tolerated without adverse effects.

“We think that with the foam used in this study, we’re not even coming close to the levels that we would be concerned about,” Otterbein said. “What we have learned from the inhaled gas trials has paved a path to say it’s safe, as long as you know and can control how much you’re giving, much like any medication. That’s another nice aspect of this approach—we can control the exact dose.”
As part of their reported study, the researchers also created carbon monoxide-containing gels, as well as gas-filled solids, using techniques similar to those used to make Pop Rocks, the hard candies that contain pressurized carbon dioxide bubbles. “ … we showed that administration of CO through foam, solid, and hydrogel GEMs can deliver titratable amounts of CO locally and systemically,” they wrote. “We demonstrated that formulations enabling the administration of CO through noninhaled routes are tunable and not limited by delivery materials, toxicity, or potency. Our preclinical results suggest that delivery of CO through these materials is dose dependent and tunable and very amenable to rectal administration.”
The team plans to test the different formulations in further studies, in addition to developing foams that might be suitable for tests in human patients. The CO delivery systems could also be used alongside other therapies, they suggested. “ … our systems are amenable to coadministration with other therapies to improve treatment efficacy, such as in concert with powdered drug formulations.”
The team pointed out that further improvements in the system that might increase CO content further, or the use of GEMs with other gases, such as nitric oxide or hydrogen sulfide, could further expand utility of the technology. “In summary, our innovative approach using safe materials will offer modalities for the administration of therapeutic gases and treatment of acute and chronic inflammatory disorders,” they wrote. “Given the broad therapeutic benefits of CO, the GEMs described may be adopted for not only many different clinical applications, particularly inflammation-mediated GI conditions, but also pathologies as diverse as cancer, ileus, trauma, and organ transplant, among others.”





