To ensure the health of the cell’s protein herds, the ubiquitination system marks misfolded or damaged proteins for destruction. But the ubiquitination system can be overzealous, targeting proteins that are less than perfect, but still able to carry out their usual, useful functions. Conceivably, if less-than-perfect proteins were to be spared, they could serve therapeutic purposes.
This possibility is being explored by scientists based at Columbia University. They are developing engineered deubiquitinases (enDUBs) that can reverse the ubiquitination system’s ruthless machinations. Importantly, the enDUBs can discriminate between proteins that should be spared, and those that really do need to be destroyed.
Details of this work recently appeared in Nature Methods, in an article titled, “Targeted deubiquitination rescues distinct trafficking-deficient ion channelopathies.” This article describes how the Columbia scientists’ approach, which relies on a new technology that incorporates synthetic llama antibodies, could be used to treat dozens of diseases, including cystic fibrosis, that arise from the destruction of imperfect but still perfectly functional proteins.
“We developed enDUBs that enable selective ubiquitin chain removal from target proteins to rescue the functional expression of disparate mutant ion channels that underlie long QT syndrome (LQT) and cystic fibrosis (CF),” the article’s authors wrote. “In an LQT type 1 (LQT1) cardiomyocyte model, enDUB treatment restored delayed rectifier potassium currents and normalized action potential duration. CF-targeted enDUBs synergistically rescued common and pharmacotherapy-resistant CF mutations when combined with [drugs that have already been approved by the FDA].”
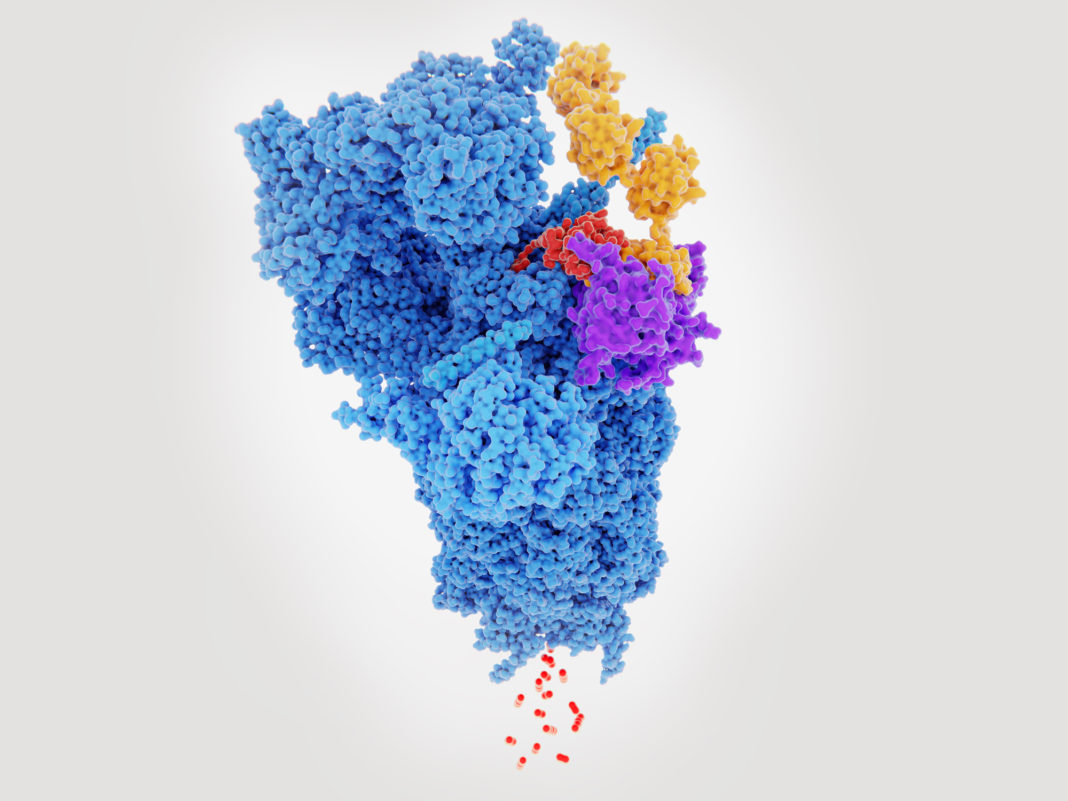
The enDUBs are modified deubiquitinases. Like ordinary deubiquitinases, the enDUBs remove the ubiquitin tags—small peptides that say “destroy me”—that are applied by the ubiquitination system. The enDUBs, however, incorporate a synthetic nanobody that recognizes a specific protein.
Natural nanobodies are small antibodies produced by llamas, camels, and alpacas. These molecules, which were discovered nearly 30 years ago, bind their targets with exquisite specificity and retain this property inside cells, unlike regular antibodies.
In the current study, nanobodies were produced that recognized and bound only selected targets. One of the targets was a protein mutated in CF. The other was a protein mutated in LQT syndrome, an inherited heart disease that can cause arrhythmia and sudden death.
“Altogether,” the authors of the Nature Medicine article asserted, “targeted deubiquitination via enDUBs provides a powerful protein stabilization method that not only corrects diverse diseases caused by impaired ion channel trafficking, but also introduces a new tool for deconstructing the ubiquitin code in situ.”
The Columbia team, which was led by Henry Colecraft, PhD, also noted that deploying enDUBs should be more effective than simply increasing DUB activity and indiscriminately rescuing all proteins in a cell marked for destruction. Suspending all protein destruction in the cell would be harmful.
Colecraft observed that in many genetic diseases, including cystic fibrosis, mutated proteins are capable of performing their jobs but are tagged for destruction by the cell’s quality control mechanisms. “The situation is analogous to ugly fruit,” he said. “Shoppers reject fruit that doesn’t look perfect, even though ugly fruit is just as nutritious. If mutated proteins in cystic fibrosis can escape the cell’s quality control mechanisms, they work pretty well.”
“A lot of proteins are destroyed by the cell for good reason,” Colecraft added, “so a therapy needs to be selective.”
To build each enDUB, Colecraft and colleagues, including graduate student, Scott Kanner, first had to find the right nanobody. Until recently, researchers had to inject their target proteins into llamas, camels, or alpacas and wait for the animal to generate such nanobodies. The Columbia researchers instead fished out binders from a synthetic yeast nanobody display library containing millions of unique nanobodies.
Once created, each enDUB was tested in cells that produced the mutated proteins.
In both cases, enDUBs prevented the destruction of the proteins, and the proteins migrated to their normal locations in the cell membrane where they performed their normal functions.
“In the case of one of the cystic fibrosis proteins we tested, we get a remarkable rescue, restoring protein levels in the cell membrane to about 50% of normal,” Colecraft reported. “If that happened in a patient, it would be transformative.”
Though both diseases investigated in the study are caused by mutations in ion channel proteins, “the approach can be applied to any protein in the cell, not just membrane proteins or proteins altered by genetic mutations,” Colecraft maintained. “It could be applicable to any disease where protein degradation is a factor, including cancer and epilepsy.”