Graft-versus-host disease (GvHD) is a potentially life-threatening medical condition that is common after allogeneic hematopoietic stem cell transplantation (HSCT), the only curative treatment for various types of leukemias. In GvHD, white blood cells from transplant donor recognize recipient cells as non-self and attack recipient tissues. Understanding how these donor white blood cells remain active against recipient cells can pave the way for novel treatment strategies in GvHD.
Scientists at the University of Helsinki have been investigating the role of T cell mutations in GvHD. Somatic mutations during one’s lifetime are common in cancer cells, but little is known about their existence and significance in other cells, such as cells in the body’s defense system.
In an article “Somatic mTOR mutation in clonally expanded T lymphocytes associated with chronic graft versus host disease” published in Nature Communications, the study first identified an index chronic GvHD patient with an activating somatic mutation in a gene called mTOR, which regulates cell growth and cell survival. The authors then screened an international cohort of 135 GvHD patients and 54 healthy blood donors. By using next generation sequencing, the scientists found that 2.2% of chronic GvHD patients, but none of the healthy blood donors, harbored a mutation in mTOR.
“Here we report studies of a patient with chronic GvHD (cGvHD) carrying persistent CD4+ T cell clonal expansion harboring somatic mTOR, NFKB2, and TLR2 mutations. In the screening cohort (n = 134), we detect the mTOR P2229R kinase domain mutation in two additional cGvHD patients, but not in healthy or HSCT patients without cGvHD,” write the investigators.
“Functional analyses of the mTOR mutation indicate a gain-of-function alteration and activation of both mTORC1 and mTORC2 signaling pathways, leading to increased cell proliferation and decreased apoptosis. Single-cell RNA sequencing and real-time impedance measurements support increased cytotoxicity of mutated CD4+ T cells. High throughput drug-sensitivity testing suggests that mutations induce resistance to mTOR inhibitors but increase sensitivity for HSP90 inhibitors. Our findings imply that somatic mutations may contribute to aberrant T cell proliferations and persistent immune activation in cGvHD, thereby paving the way for targeted therapies.”
“What makes our finding particularly significant is that the mutation now found was recurrent, meaning that the same mutation was found in several patients with chronic GvHD,” says Satu Mustjoki, MD, PhD. “Our previous studies in rheumatoid arthritis had shown that acquired mutations could be found in T cells, but in these studies, the mutations had been isolated and the same mutations had not been found in more than one patient.”
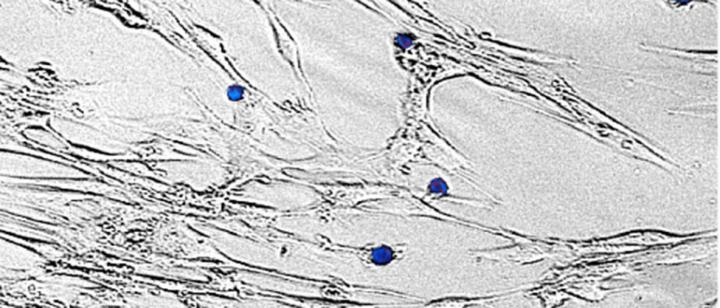
Using single-cell RNA sequencing and T cell receptor sequencing on samples collected from the index patient, researchers found that the mTOR mutated CD4+ T cell clone expanded during the course of GvHD despite immunosuppressive treatment, suggesting the mutation contributed to the disease pathogenesis. In addition, it was found that the mutation was located in so-called cytotoxic T cells and these cells were able to damage the body’s own cells. Researchers also investigated the mTOR mutation in more detail by introducing it into a human cell line. The activating mTOR mutation promoted cell proliferation and cell survival.
The researchers performed a high-throughput drug screen with 527 drugs to identify potential targeted therapies. The index patients’ CD4+ T cells were sensitive to a specific class of drugs called HSP90 inhibitors, suggesting that these drugs could be used to treat GvHD in the future.
“Our study helps to understand the mechanisms of activation of the immune system in GvHD. Although several different drug combinations have been tried in the treatment of GvHD, using our results, it is possible to find individualized treatments for patients,” says doctoral candidate Daehong Kim from the University of Helsinki.
Further studies using larger cohorts of GvHD are warranted to understand whether clonal mutations in T cells modify GvHD severity, drug responses, and clinical outcome.