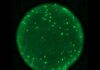
Paper in Diabetes describes the PANIC-ATTAC mouse, which can be used to study inducible and reversible beta-cell ablation.
UT Southwestern Medical Center researchers have genetically engineered a lab mouse to regenerate pancreatic beta cells that have been induced to die, mimicking type 1 and 2 diabetes.
The scientists genetically manipulated mature, insulin-positive pancreatic beta cells in the PANIC-ATTAC mice, so that these cells would die when they came in contact with a drug. When the researchers stopped administering the drug and allowed the animals to recover, they found that their beta cells regenerated and their blood glucose levels returned to normal after two months.
“This model allows us to get a transcriptional signature, a fingerprint, of how beta cells fend off the pharmaceutical stimulus we provide to prompt cell death,” Dr. Scherer explains. “In other words, it provides a way to identify the most critical factors that protect against beta-cell death and to potentially find ways to increase these factors in people with type 1 diabetes.”
The key, according to Dr. Scherer, is that the process used to kill beta cells is targeted. “It creates very little inflammation, so we can eliminate specific cells with minimal collateral damage. The other nice aspect is that we can do it in a very dose-dependent way, so we can ablate, or kill, just a few cells or we can ablate almost all of them.”
Dr. Scherer says that this model lends itself to studying conditions of temporary hyperglycemia such as gestational diabetes, a condition in which pregnant women who have never had diabetes develop hyperglycemia.
The PANIC-ATTAC mouse may also be used to test how specific pharmaceuticals impact beta-cell regeneration, reports Zhao Wang, Ph.D., a postdoctoral researcher at UT Southwestern and lead author of the study. “We can test which drugs can more rapidly repair the damage. We can also test which drugs are protective. That’s probably more important physiologically because it allows us to screen for interventions that could protect beta cells during the early stages of diabetes to slow down and prevent the onset of hyperglycemia.”
It’s unclear what caused the pancreatic beta cells to regenerate, notes Philipp Scherer, Ph.D., professor of internal medicine, director of the Touchstone Center for Diabetes Research at UT Southwestern, and senior author of the study. Dr. Schere and colleagues are now developing a way to isolate the cell population that gives rise to the newly emerging beta cells.
Besides other researchers from UT Southwestern, scientists from the Albert Einstein College of Medicine and Merck Research Laboratories also participated in this study.
The animal model is described online in the journal Diabetes.