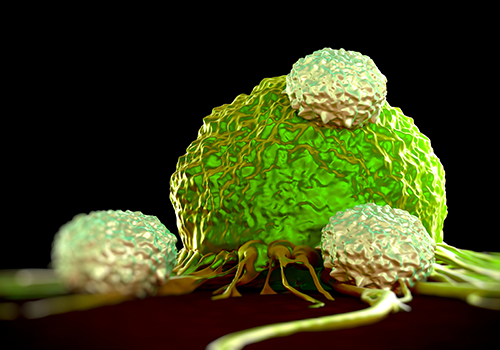
![PD-L2 protein expression in human tumors was associated with clinical response to pembrolizumab (Keytruda®), an anti-PD-1 immunotherapy, independent of PD-L1 expression, in patients with head and neck squamous cell carcinoma (HNSCC) [royaltystockphoto/Getty Images]](https://genengnews.com/wp-content/uploads/2018/08/Jun15_2017_Getty_486569844_TCellAttackingCancer_5002553221382-1.jpg)
PD-L2 protein expression in human tumors was associated with clinical response to pembrolizumab (Keytruda®), an anti-PD-1 immunotherapy, independent of PD-L1 expression, in patients with head and neck squamous cell carcinoma (HNSCC) [royaltystockphoto/Getty Images]
Immunotherapy has ignited a firestorm of interest from scientists to the media, as many of the therapeutic compounds in this class have proven successful at combating disease like cancer when many other drugs have failed. Much of immunotherapy research from the past several years has been centered around one (PD-L1, or programmed death-ligand 1) of the two ligands for the programmed cell death receptor, programmed cell death protein 1 (PD-1). However now, a team of investigators led by scientists at Merck Research Laboratories has just released their findings that PD-L2 protein expression in human tumors was associated with clinical response to pembrolizumab (Keytruda®), an anti-PD-1 immunotherapy, independent of PD-L1 expression, in patients with head and neck squamous cell carcinoma (HNSCC).
The findings from this new study were published recently in Clinical Cancer Research through an article entitled “PD-L2 Expression in Human Tumors: Relevance to Anti-PD-1 Therapy in Cancer.”
“It is well known that PD-1 has two binding partners, PD-L1 and PD-L2, yet most of the published work to date has looked at the distribution and predictive benefits of PD-L1 expression alone,” explained senior study investigator Jennifer Yearley, D.V.M., Ph.D., senior principal scientist of anatomic pathology at Merck Research Laboratories. “We developed an assay that detects PD-L2 with a high degree of specificity and sensitivity to evaluate the prevalence of PD-L2 in human tumors and assess the relationship of PD-L2 expression with clinical response to pembrolizumab in patients with HNSCC.”
In the new study, the research team analyzed over 400 archival tumor samples across seven cancer types (renal cell carcinoma, bladder, melanoma, non-small-cell lung cancer, triple-negative breast cancer, gastric carcinoma, and HNSCC) with the novel immunohistochemistry assay. “We were very surprised to find how common PD-L2 expression was across all of the tumor types we evaluated,” Dr. Yearley noted.
Interestingly, the scientists found that PD-L2 expression varied significantly among tumor types. For instance, gastric cancer and triple-negative breast cancer showed moderate to elevated levels of expression, whereas expression in renal cell carcinoma was predominantly low. Additionally, over half of the HNSCC samples showed tumor cell expression of PD-L2, while tumor cell expression was not seen in any of the renal cell carcinoma and very few of the melanoma samples.
Based on their findings, the investigators took to analyzing tumor samples from 172 patients with recurrent or metastatic HNSCC in two combined cohorts who had been assigned treatment with pembrolizumab during the KEYNOTE-012 trial. The scientists found that clinical response was related to the expression of PD-L2, suggesting that therapy targeting both PD-L1 and PD-L2 may enhance patient response.
“The overall response rate (ORR) for the two KEYNOTE-012 cohorts in this study was 27.5% among patients whose tumors were positive for both PD-L1 and PD-L2, more than two times higher than the 11.4% ORR for patients whose tumors were positive only for PD-L1,” Dr. Yearley remarked.
Ongoing studies are focusing on the expression of PD-L2 along with PD-L1 and other immune-related analytes, which are included in a gene expression profile that reflects a T-cell inflamed tumor microenvironment. This profile has been shown to be related to response to anti-PD-1 therapy and is currently being evaluated for potential diagnostic use in pembrolizumab clinical trials.
The authors noted that, overall, this study suggests that PD-L2 expression may provide additional information beyond PD-L1 positivity in predicting clinical response to anti-PD-1 therapies.