In with the new and out with the old, goes the classic phrase, but it’s an action we do on average every four seconds that most of us take for granted as we inhale the new and expel the spent air. This simple action typically goes unnoticed and keeps us alive, but for the millions of people suffering from respiratory diseases, breathing is an omnipresent concern. For decades, scientists have looked for ways to recapitulate the complex nature of lung tissue, with the hope that they could provide a better understanding of diseases affecting the lungs.
Now, a team of researchers led by investigators at Columbia University Medical Center (CUMC) has recently reported on new lung organoids, tiny 3D structures that mimic features of a full-sized lung, that have been created from human pluripotent stem cells. In the new study—published recently in Nature Cell Biology in an article entitled “A Three-Dimensional Model of Human Lung Development and Disease from Pluripotent Stem Cells”—the researchers used the organoids to generate models of human lung diseases in vitro, which they are optimistic will advance our understanding of a variety of respiratory diseases.
“Researchers have taken up the challenge of creating organoids to help us understand and treat a variety of diseases,” explained senior study author Hans-Willem Snoeck, Ph.D., professor of medicine at CUMC. “But we have been tested by our limited ability to create organoids that can replicate key features of human disease.”
Organoids are 3D structures containing multiple cell types that look and function like a full-sized organ. By reproducing an organ in a dish, researchers hope to develop better models of human diseases and find new ways of testing drugs and regenerating damaged tissue.
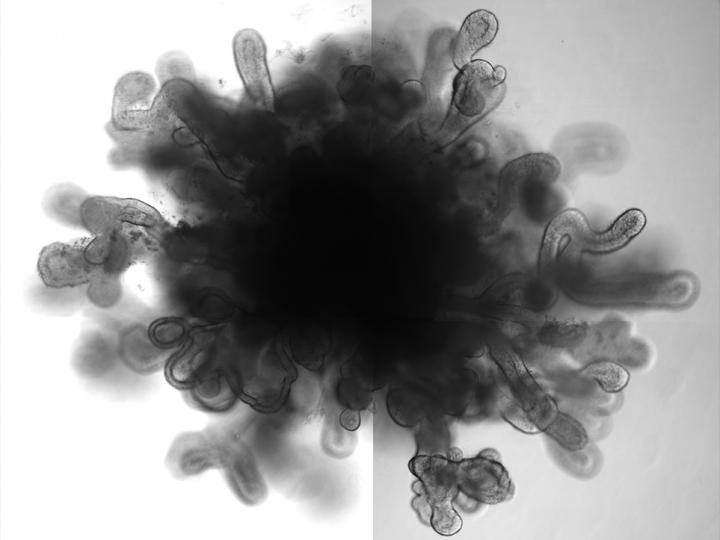
Researchers at Columbia University Medical Center have developed three-dimensional lung bud “organoids” from human pluripotent stem cells. The “mini organs” could be used to model lung diseases such as pulmonary fibrosis and respiratory syncytial virus infection. [Columbia Medicine].
Amazingly, Dr. Snoeck and his colleagues were able to generate lung organoids in the lab that are the first to include branching airway and alveolar structures, similar to human lungs. To demonstrate their functionality, the researchers showed that the organoids reacted in much the same way as a real lung does when infected with respiratory syncytial virus (RSV). “We report here the generation of hPSCs [human pluripotent stem cells] of lung bud organoids (LBOs) that contain mesoderm and pulmonary endoderm and develop into branching airway and early alveolar structures after xenotransplantation and in Matrigel 3D culture,” the authors wrote. “Expression analysis and structural features indicated that the branching structures reached the second trimester of human gestation. Infection in vitro with respiratory syncytial virus, which causes small airway obstruction and bronchiolitis in infants, led to swelling, detachment and shedding of infected cells into the organoid lumens, similar to what has been observed in human lungs.”
RSV is a major cause of lower respiratory tract infection in infants and has no vaccine or effective antiviral therapy. Additional experiments revealed that the organoids also responded as a human lung would when carrying a gene mutation linked to pulmonary fibrosis.
“Introduction of mutation in HPS1, which causes an early-onset form of intractable pulmonary fibrosis, led to the accumulation of extracellular matrix and mesenchymal cells, suggesting the potential use of this model to recapitulate fibrotic lung disease in vitro,” the authors stated. “LBOs therefore recapitulate lung development and may provide a useful tool to model lung disease.”
Idiopathic pulmonary fibrosis, a condition that causes scarring in the lungs, causes 30,000 to 40,000 deaths in the U.S. each year. A lung transplant is the only cure for this condition.
“Organoids, created with human pluripotent or genome-edited embryonic stem cells, may be the best, and perhaps only, way to gain insight into the pathogenesis of these diseases,” Dr. Snoeck concluded.