![Cancer cells move through newly developed microfluidic chamber. [Michigan Medicine]](https://genengnews.com/wp-content/uploads/2018/08/149704_web1972541711-1.jpg)
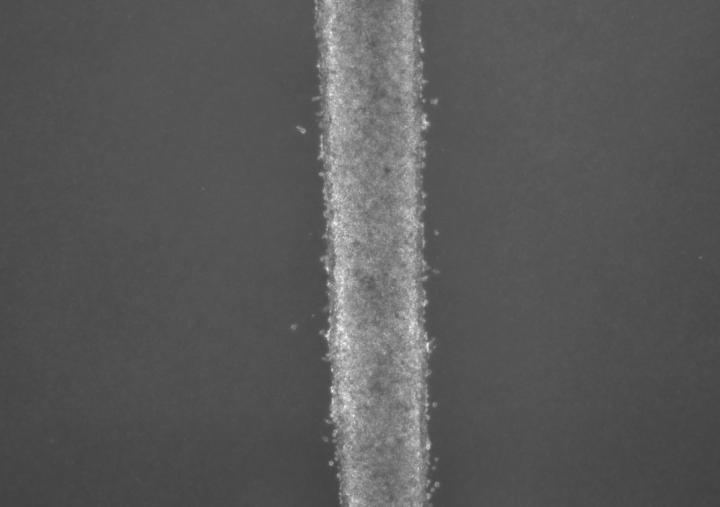
Cancer cells move through newly developed microfluidic chamber. [Michigan Medicine]
The fog of war is often described by strategists as the level of uncertainty in situational awareness during military operations. Knowing where and when your enemy will attack would, at the very least, offer the opportunity to bolster defenses, if not prevent the incursion altogether. Now, investigators at the University of Michigan have just created a fluidic device that looks to track the early cancer aggressor cells—helping to lift the fog in the war on cancer. Findings from the new study were published today in Scientific Reports, in an article entitled “Tracking the Tumor Invasion Front Using Long-Term Fluidic Tumoroid Culture.”
“It's especially important to be able to capture those leader cells and understand their biology—why are they so successful, why are they resistant to traditional chemotherapy, and how can we target them selectively?” explained co-senior study investigator Sofia Merajver, M.D., Ph.D., scientific director of the breast oncology program at the University of Michigan Comprehensive Cancer Center. “Microfluidic devices are helping us understand biology that was previously not accessible.”
A current drawback of existing microfluidic devices is that the cells don't last long within them. These devices typically lend themselves to brief experiments of several days. However, the characteristics of cancer cells change over time.
“A lot of tumor processes, like invasion and resistance, don't happen overnight. Our goal was to track the long-term evolution of invasion,” noted lead study investigator Koh Meng Aw Yong, Ph.D., a postdoctoral fellow in Dr. Merajver's lab. “We cannot look at just a certain time point, like in a three-day experiment. That might not represent what's happening in the body over time.”
With that focus in mind, the researchers developed a new fluidic device that allows them to cultivate cells for longer periods of time. The team found that the device was stable for up to at least three weeks in culture. The cells look like a thin milky line in a chamber that's smaller than a pill box. They are suspended in three dimensions, unlike typical fluidic devices that capture cells in two dimensions. It allows researchers to feed the cancer cells into the device with very minimal disturbance or change to the cells.
Interestingly, the microfluidic device consists of three tiny molded channels through which cells flow. The cells are fed into one channel. Fluid flows through a parallel channel to provide pressure and flow without disturbing the culture. The flow of fluid through the outer channel mimics what happens with the body's capillaries.
“These forces are important and incorporate everything into one system,” Dr. Aw Yong remarked.
The Michigan team tested the device with two lines of metastatic prostate cancer cells. They were able to isolate the leader cells—those cells that first broke off and would be traveling to distant organs. After two weeks, the investigators found that the cells from one line were twice as invasive as the other cell line. But by three weeks, that difference was gone, suggesting that the invasive potential of cells may change over time.
“We [show that] a fluidic device for a long-term three-dimensional tumoroid culture which recapitulated the tumor invasion front, allowing for both quantification of invasive potential and molecular characterization of invasive leader cells,” the authors wrote. “Preliminary analysis of the invasion front indicated an association with cell proliferation and higher expression of growth differentiation factor 15 (GDF15). This device makes real-time tracking of invading leader cell phenotypes possible and has potential for use with patient material for clinical risk stratification and personalized medicine.”
Dr. Merajver and her colleagues are optimistic that they can find differences in the molecular signature between cells that invade and those that don't. Then, they would target the molecular underpinning with therapies to prevent cancer from invading—essentially keeping the cancer confined and preventing metastasis.
“The device also holds potential to be used to test drugs and detect when cancer becomes resistant. This would allow oncologists to know sooner if a therapy is not working, and perhaps switch the patient to another option,” commented co-senior study investigator Jianping Fu, Ph.D., associate professor of mechanical engineering at the University of Michigan. “Of course, more research is needed to explore this possibility in the future.”
The research team is looking to extend their work to triple-negative breast cancer, a particularly aggressive form of the disease. Once the leader cells are identified, they will also begin looking at whether these cells have different genetic or molecular markers than the less-aggressive cells.
“We think we can grow this while the patient is undergoing treatment or monitoring,” Dr. Aw Yong concluded. “The device would be able to show us if the cells become more aggressive before a traditional imaging test would detect anything.”