April 1, 2012 (Vol. 32, No. 7)
Medulloblastoma, the Most Malignant Brain Cancer in Children, Is One Current Focus
The California Institute for Regenerative Medicine (CIRM), a state granting agency created by a voter-approved ballot initiative in 2004, gave $43 million toward the construction of a new research facility that just opened its doors last fall in the Torrey Pines Mesa research cluster in San Diego’s La Jolla region.
The building, known as the Sanford Consortium for Regenerative Medicine, is thought of as a “collaboratory,” rather than a new stand-alone research institution. Here, scientists from five local research institutes—Sanford-Burnham Medical Research Institute, the University of California, San Diego, The Scripps Research Institute, the Salk Institute, and La Jolla Institute for Allergy and Immunology—are relocating their laboratories to a space specifically designed to spur collaboration.
One of these Sanford Consortium collaborators is Robert Wechsler-Reya, Ph.D. In 2010, Dr. Wechsler-Reya became the first recipient of a $5.9 million CIRM Leadership Research award. These awards were meant to help California institutions attract top-notch stem cell scientists to the state, and that’s what it did. Dr. Wechsler-Reya is now a professor and program director at Sanford-Burnham Medical Research Institute in La Jolla and his wife, Tannishtha Reya, Ph.D., also a stem cell researcher, is a professor at nearby UC San Diego.
Touching on stem cell biology, tumor development, and drug discovery, Dr. Wechsler-Reya’s research is a good representation of work that will be coming out of the Sanford Consortium collaboratory. His lab was the first to identify a new type of stem cell that, when functioning normally, develops into many different cell types in the cerebellum. But if this cell acquires certain mutations, it can also give rise to medulloblastoma, the most common malignant brain cancer in children.
Dr. Wechsler-Reya’s team is now trying to better understand what drives medulloblastoma tumors, and they are creating stem cell-based models that can be used to test new drugs that target the disease.
In a study published February 13 in Cancer Cell, Dr. Wechsler-Reya and his group developed a new mouse model for studying medulloblastoma. The model mimics the deadliest of four subtypes of the human disease, a tumor that is triggered by elevated levels of the Myc oncogene.
Using this model, the team profiled gene expression in Myc-driven medulloblastoma tumors. They found particularly high levels of genes activated by PI3-kinase, an enzyme whose activity is often elevated in cancer cells. Armed with this information, the team tested whether inhibiting PI3-kinase could block the growth of these Myc tumors. They found that PI3-kinase inhibitors significantly increased mouse survival.
PI3-kinase inhibitors are in clinical trials for several types of cancer, but no one has tried them as a treatment for medulloblastoma. Dr. Wechsler-Reya’s lab is now taking steps toward testing these inhibitors as a potential therapy for the disease.
“The key is to take compounds that show promise in preclinical studies in the lab and partner with clinicians to evaluate their effectiveness in the clinic,” Dr. Wechsler-Reya said. “Our hope is that this approach will bring new therapies to children who are suffering from this extremely aggressive disease.”
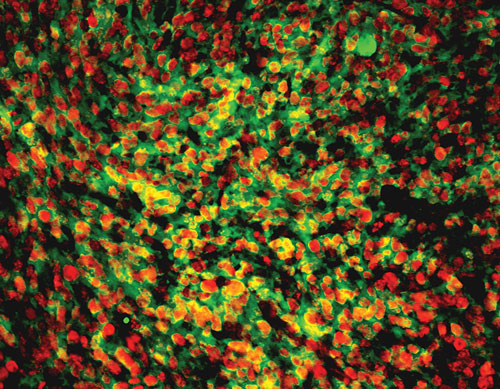
Cerebellar stem cells engineered to express Myc and mutant p53 (shown here) give rise to aggressive tumors that resemble a particularly malignant form of human medulloblastoma, providing a new model that will help scientists develop more effective therapies for this disease.







